Key messages
In the adult population the use of oral nutrition supplements within the hospital setting allows to alleviate the malnutrition. However, only limited research has been done to quantify benefits of interventional nutrition care.
After the consumption of oral nutritional supplements, an increased energy (25%) and protein (32%) consumption was shown with appropriate tolerance. This can contribute to contrast low intake that occurs and thus prevent or treat malnutrition.
The findings demonstrate that oral nutrition supplements be a good tool to impact the nutritional adequacy. Individualized early implementation of nutrition therapy for malnourished patients can led to fewer complications rates.
Introduction
The European Society for Clinical Nutrition and Metabolism (ESPEN) defines the disease-related malnutrition as a weight loss related to the disease or a deficit in specific nutrients1, the prevalence varies between 20-50% in hospitalized adults. The malnutrition etiology can be given by increased catabolism, a low nourishment and energy supply that could be secondary to a low intake and/or the decreased nourishment absorption2.
Within this last item, decreased oral intake during hospital stay has been documented as a risk factor associated to malnutrition (OR=3.07, CI95%: 1.84-5.1, p<0.001)3. However, the use of oral nutrition supplements (ONS) within the hospital setting allows to alleviate the malnutrition burden having as an impact decreased hospital stay days, even though frequently this support is during relatively short periods, due to a great variety of ONS, they are adapted to specific clinical conditions.
The use of ONS in patients with disease-related malnutrition reduces significantly the hospital readmissions as compared to the routine care (OR=0.59, CI95%: 0.43-0.80, p=0.001)4. Therefore, produces profitable outcomes, and cost savings, reporting a 12.2% in patients with abdominal surgery (p=0.027)5 and prevented the development of 2,896±632 pressure ulcer cases per year, while releasing 12,396±4991 bed days, which translated in €2,869,526±2,078,715 per year in savings6. The objective of this study was to assess the risk of hospital malnutrition and the effect of ONS during 4 days in anthropometric variables, energy and protein nourishment consumption in patients admitted in a third-level hospital.
Methodology
A cohort study was carried out in a third-level hospital in Mexico City during one month (April 2018), in which the consecutive patient was admitted. The eligible adult patients that were admitted to the hospitalization area; as exclusion criteria: critical patients, presence of chronic kidney and hepatic disease, with exacerbated or active intestinal inflammatory disease, with nutrition support at admission. His/her malnutrition risk on admission using the tool Nutritional Risk Screening-2002 (NRS-2002)7, and nutrition status were assessed (for dietitian nutritionists and physician nutrition specialist members of clinical nutrition service.
The anthropometric measures were taken with an electronic scale (8721321959; SECA) for the body weight; the height was measured with a wall-mounted stadiometer (tape Lufkin executive thinline W606P) and for those patients that could not stand up, the formulas knee-heel length (KHL)8 were used to calculate the height; the Chumlea formula was used to predict weight and height9. The muscle strength estimated with hand dynamometry was measured with a dynamometer (Takei® 5401)10.
The intake balance was collected by a multiple-step 24-hour recall11; in which the quantity of food that was consumed by the patients in 24 hours was recorded, and afterwards a caloric count was carried out reporting grams of carbohydrates, proteins, and lipids, and total kilocalories. The adequacy percentage was calculated considering the caloric and protein requirement calculated from the fast formula outlined by American Society for Parenteral and Enteral Nutrition (ASPEN)12 and National Institute and Care Excellence (NICE)13 guidelines, taking this value as 100%, was taken as an appropriate intake value of ≥80% of the recommendation14.
The ONS prescription was observed and there was a 4-day follow-up; during this period of time, the consumed energy and protein intake was assessed. The patients were asked about their consumption and it was confirmed with the quantity of product in the cans measured as a percentage remaining; also, the patient was asked as an open question if the ONS consumption caused any gastrointestinal symptoms, e. g.: bloating, diarrhea, nausea, vomiting, constipation.
The variable distribution was determined using the Kolmogorov-Smirnov statistical test. The quantitative variables were expressed as average ±standard deviation and the qualitative variables as percentage. To compare the baseline vs final measurements a paired t test was used or the statistics Xi2 as per the variable type. To compare the variables of those that consumed ONS vs. those who did not, the T Student statistics were used for independent samples. The significant value of p was established <0.05. The data was analyzed by the SPSS program (version 25, SPSS Inc, Chicago, IL.). This study was approved (number 2119) by the Institution's Ethics and Research Committees.
Results
A total of 290 patients (167W/123M) were included, 10.3% (n=30) were prescribed with ONS, and the remaining 89.7% (n=260) were not prescribed with ONS. The patients that had an ONS prescription showed significantly more malnutrition (less body weight, BMI, muscle strength, as well as a higher percentage of malnutrition risk on admission) (Table 1).
Table 1. Baseline Characteristics Stratified by Who Received ONS.
| Without ONS n=260 | With ONS n=30 | p | |
|---|---|---|---|
| Age (years) | 54 ± 19 | 55 ± 21 | 0.819 |
| Weight (kg) | 67.5 ± 15 | 53 ± 11.5 | < 0.0001 |
| BMI (kg/m2) | 25.7 ± 5.3 | 21.3 ± 4.5 | < 0.0001 |
| Muscular strength (kg) | 17.7 ± 10 | 12.6 ± 9 | 0.009 |
| Consumed energy (kcal) | 1218 ± 417 | 1079 ± 507 | 0.104 |
| Consumed energy (g/kg of bodily weight) | 19 ± 7 | 21 ± 10 | 0.314 |
| Consumed protein (g) | 53.9 ± 25 | 50 ± 27 | 0.406 |
| Consumed protein (g/kg of bodily weight) | 0.8 ± 0.4 | 0.9 ± 0.5 | 0.168 |
| Energy adequacy (%) | 77.7 ± 28 | 73.2 ± 32 | 0.434 |
| Protein adequacy (%) | 68. 3 ± 35 | 76 ± 42 | 0.245 |
| Risk of malnutrition NRS, score | 2 ± 1.9 | 3.4 ± 1.8 | < 0.0001 |
| *Risk of malnutrition NRS, n (%) | 121 (46.5) | 25 (83.8) | < 0.0001 |
| Diagnoses, n (%) | |||
| Respiratory | 3 (1.2) | 0 (0) | |
| Gastrointestinal | 50 (19.2) | 5 (16.7) | |
| Neurology | 9 (3.5) | 0 (0) | |
| Oncology | 86 (33) | 6 (20) | |
| Infectiology | 63 (24.3) | 13 (43.3) | |
| Others | 49 (18.8) | 6 (20) | |
BMI: Body mass index; NRS: Nutrition risk assessment; ONS: Oral nutritional support.
T statistic analysis of independent samples,
*Xi2.
The participants who received ONS, 58.6% received hyperenergetic formula, 17.2% standard formula, 13.8% formula to improve glycemic control, and 10.4% other formulas. Of patients included 66.6% had a ≥50% ONS consumption during the 4 days they were observed, because they did not like the taste, lost their appetite or presented some gastrointestinal symptoms. According to the presence of gastrointestinal symptoms during the follow-up of ONS consumption, the first and second day, 90.1% did not show symptoms and on day 3 and 4, 96.7%. A patient showed appetite loss throughout the follow-up; another patient reported abdominal distention on days 1 and 2, but not for days 3 and 4. Finally, another patient showed diarrhea the first two days but did not report any symptoms on days 3 and 4.
After the consumption of ONS, the participants showed a significant increase in consumed and in the energy adequacy percentage; on the baseline, 44.8% of the subjects that received ONS showed a <65% calorie adequacy percentage and 37.9% of the participants showed a ≥80% calorie adequacy percentage. For the baseline protein adequacy percentage, 41.4% of the patients that received ONS showed a <65% adequacy percentage and 44.8% of the participants showed a ≥80% protein adequacy percentage.
The proportion of subjects with a <65% calorie adequacy decreased to 21.5% and the proportion of participants with a ≥80% calorie adequacy percentage increased to 60.7% at the end of the 4-day follow-up. The proportion of subjects with a <65% protein adequacy percentage decreased to 21.4% and the proportion of participants with a ≥80% protein adequacy percentage increased to 53.6% (Figure 1). However, an important concern in this type of interventions is the adherence to the ONS consumption, therefore, the analysis was carried out in those that during the 4-day consumption had a ≥50% ONS adherence and it was documented that 66.6% of the participants had adherence during follow-up.
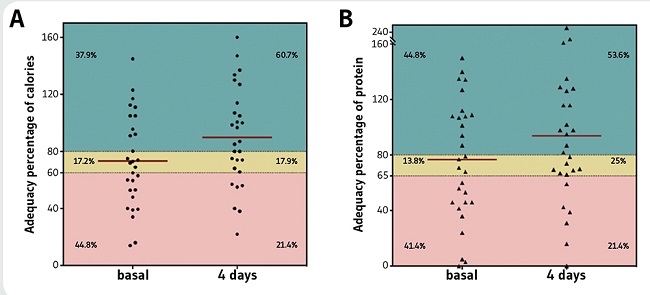
Figure 1. Percentage of Ingested Calorie and Protein Adequacy, Before and 4 Days After the ONS Consumption.
When analyzing only the patients with adherence, we observed a significant increase in the energy consumption, taking the energy adequacy percentage from 73.6±33% to 101±32% (p=0.003). Similarly, a significant increase in the protein consumption was observed, which increased the adequacy an average of 75.8±45% to 108 ± 58% (p=0.016) (Figure 1).
No changes were found in anthropometric variables or in arm strength when comparing baseline and at day 4 measurements when analyzing all patients or only those who consumed ≥50% of the ONS (Table 2).
Table 2. Assessment After the 4 Days in Which Patients Received ONS.
| Variables | All that received ONS (n=30) | Patients that received ONS with a ≥50% consumption adherence (n=20) | ||||
|---|---|---|---|---|---|---|
| Baseline | 4 days | p | Baseline | 4 days | p | |
| Weight (kg) | 53 ± 11.5 | 52.5 ± 11 | 0.305 | 50.4 ± 11 | 49.8 ± 10.9 | 0.556 |
| BMI (kg/m2) | 21.3 ± 4.5 | 20.8 ± 3.9 | 0.250 | 21.4 ± 4.4 | 20.8 ± 3.9 | 0.574 |
| Muscular strength (kg) | 12.6 ± 9 | 12.5 ± 9 | 0.866 | 12.5 ± 9.2 | 12.2 ± 9.9 | 0.719 |
| Consumed energy (kcal) | 1079 ± 507 | 1287 ± 433 | 0.035 | 1039 ± 458 | 1422 ± 395 | 0.004 |
| Consumed protein (g) | 50 ± 27 | 68 ± 28 | 0.098 | 47.4 ± 27 | 79.4 ± 53.5 | 0.047 |
| Consumed energy (g/kg weight) | 21 ± 10 | 24.9 ± 11 | 0.075 | 22.6 ± 10 | 30.3 ± 9.8 | 0.022 |
| Consumed protein (g/kg weight) | 0.9 ± 0.5 | 1.3 ± 1 | 0.137 | 1 ± 0.6 | 1.4 ± 0.7 | 0.078 |
| Energy adequacy (%) | 73.1 ± 32 | 90 ± 35 | 0.025 | 73.6 ± 33 | 101 ± 32 | 0.003 |
| Protein adequacy (%) | 76 ± 42 | 93 ± 56 | 0.05 | 75.8 ± 45 | 108 ± 58 | 0.016 |
BMI: Body mass index; ONS: Oral nutritional support.
Paired T statistical analysis.
Discussion
In this study we observed that after the follow-up of patients prescribed with ONS, the calorie consumption increased significantly. It's been considered that one of the factors that impacts the most in the onset of intrahospital malnutrition is the calorie deficit15. This calorie deficit has been related to the increased clinical complications in patients; when the accrued negative energy balance exceeded 10,000 kcal during the hospital stay, the mortality was greater than 85%16.
It is common that patients don't consume 100% of the indicated ONS, mainly due to the flavor or gastrointestinal symptoms that may arise17. In this study, although it is an important factor, the energy and protein consumed increased. It is an important finding because it is known that the protein requirement increases in hospitalized patients due to a sustained catabolism that occurs in a hypermetabolic state.
This intensifies the bodily protein decomposition, manifesting as a protein negative net balance, that can be noted clinically by the weight loss, nitrogen negative balance and skeletal muscle wear. Therefore, providing an adequate supply of dietetic protein is important in this population. However, as with the energy deficit, the protein input deficit is related with unfavorable outcomes for the patient18).
Patients with chronic diseases tend to suffer a suboptimal nutritional state secondary to their baseline pathology19. Therefore, it is important to identify early the hospitalized patients with malnutrition risk to give nutritional support customized. A third of the patients that are admitted at the hospital in developed countries have certain degree of malnutrition and among the patients that are not malnourished when admitted, a third will develop malnutrition during their hospital stay20. Hospital malnutrition is associated with substantial costs, suggesting the need to establish procedures for screening, diagnosing, and treating malnutrition21.
Therefore, the intrahospital malnutrition prevalence is highly variable, from 13-88% depending on the population type, disease type and the criteria used to identify it22,23, the prevalence found is in the range described in the literature. The disease-related malnutrition is associated to an inflammatory component and these can also increase the nutrient requirements while promoting a catabolic state24. However, the use of ONS is a tool that can be used in any hospital, to lower the complications that a patient can suffer with a suboptimal nutritional state (Figure 2). In addition to a change in diet and, if necessary, nutritional support should be initiated.
One of the limitations of the study is the design observational, sample size and the short follow-up, however the number of malnourished adult patients with adequate protein intake on 4th day of admission is a performance indicator25. However, it is worth mentioning that they did not decrease either; the follow-up was too short to observe an increased body weight. Huynh et al. observed a 2.6% increase in body weight after 4 weeks of ONS consumption, and it was greater after 12 weeks (4%)26.
Conclusions
The use of oral nutritional supplements increases considerably the energy and protein consumption in patients with a >50% adherence with appropriate tolerance, however no changes were found in anthropometric variables or in arm strength. Therefore, it proves to be a good tool to impact the nutritional adequacy.