INTRODUCTION
Deep neck infections (DNI) usually originate in pharyngeal or oral infections. It is estimated that up to 36% of cases are of dental origin [1] as a result of periodontal disease [2] periapical abscesses without or with previous dental interventions [3] or radicular cysts [4].
The microbiota of infected root canals associated with acute apical abscess is polymicrobial, composed predominantly of Gram negative anaerobes (Phylum Firmicutes and Bacteroidetes [3].
Bacteria isolated in DNI can be classified into three groups according to their relationship with the oral microbiome [1, 5]:
– Group 1: bacteria that are found in the oral microbiome and are responsible for oral pathology (caries, periodontal disease and oral infectious processes).
– Group 2: bacteria that are found in the oral microbiome but are not directly responsible for oral pathology.
– Group 3: bacteria not identified in the oral microbiome and whose culture therefore does not determine the oral origin of the DNI.
The diagnosis of DNI of dental origin is based on oral and radiological exploration and microbiological culture [1].
Objective
We present a case of DNI originated in the lower left third molar in which Prevotella buccae was isolated.
For the preparation of the case report, the CARE checklist was followed [6].
CASE REPORT
A 44-year-old Caucasian woman, with no previous medical conditions or treatments, who attended an otorhinolaryngology consultation for dysphonia with a progressive worsening of one week of evolution, without other local or general associated symptoms.
Rhinofibrolaryngoscopy showed left arytenoid edema and arytenoepiglottic fold and left hemilarynx paralysis. Normal neck. Oral treatment schedule was started with cefuroxime (500 mg / 12 h) and deflazacort (45 mg / 24 h).
Chest X-ray, cervicomediastinum computed tomography (CT) and blood analytical. The CT image showed the extension of the DNI from the left parapharyngeal space to the hypopharynx, preepiglottic space, left paraglottic space and retropharyngeal space (Figure 1).
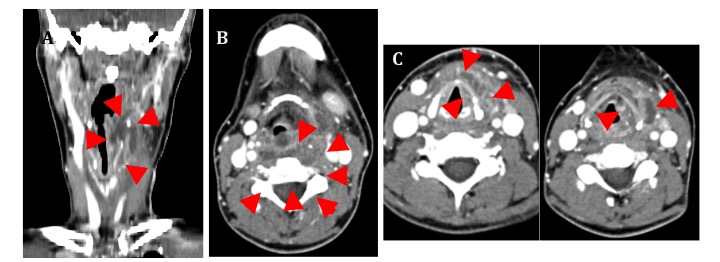
Coronal CT image (A). A. Image of the abscess that extends from the left peritonsillar and parapharyngeal space to the hypopharynx, the thyrohyoid (preepiglottic) space and the left paraglottic space. Axial CT image at the level of hyoid bone (B) and larynx (C). B. The extension of the abscess towards the left parapharyngeal, retropharyngeal and preepiglottic spaces indicated with arrows is observed. C. Abscess that affects the prethyroid area and the left paraglottic space.
Figure 1. Deep cervical abscess of dental origin.
Until the completion of the CT scan, the symptoms were progressive, requiring urgent hospital admission for dyspnea.
Left cervicotomy and drainage of the abscess were performed under general anesthesia with orotracheal intubation. Samples were taken for aerobic and anaerobic bacteria culture.
The intravenous antibiotic treatment prescribed from the emergency area was with amoxicillin / clavulanic acid 1000/200 mg (at a dose of 2 g every 8 hours). That was maintained up to ten days after the postoperative period.
The patient remained in the intensive care unit (ICU) for 3 days being extubated at 24 hours.
In the anaerobic culture, Prevotella buccae was isolated, so the patient's dental history was reviewed, which showed processes of chronic pericoronitis associated with 3.8, which could be identified in a panoramic radiograph obtained six years earlier (Figure 2). The aerobic culture was negative. Prevotella buccae was resistant to penicillin G and sensitive to amoxicillin / clavulanic acid, piperacillin / tazobactam, imipenem, clindamycin, chloramphenicol and metronidazole.

Figure 2. Panoramic radiography obtained after deep neck infection. No radiographic changes are detected in left lower third molar.
A new panoramic radiograph was performed which did not provide relevant information regarding the previous one. One month after discharge, the extraction of 3.8 was performed.
The evolution was favorable with absence of postoperative infection and recurrence of DNI after 47 months of follow-up.
DISCUSSION
Prevotella buccae is the strict anaerobic bacterium Gram negative [4] most prevalent in periodontal disease [2], it is usually present in the microflora of the mouth, the gastrointestinal tract and the vagina [7]. It is also found in oral bacterial plaque [8], in periodontal pockets in 60.4% of cases [2], in radicular cysts [4], in periapical abscesses in non-endodontically and necrotic teeth [3] and in odontogenic abscesses [3, 4,9].
Infections originate in the periapical area of the tooth and the absence of dental treatment can lead to polymicrobial cervical infections [4].
Other species have been isolated in dental and periodontal infectious diseases, such as P. denticola, P. intermedia or P. melaninogenica (39.6%, 35.4% and 22.9% respectively) [2]. Prevotella ssp is isolated in 3.6% of cultures in ICP [1]. The relative risk of finding P. buccae in an odontogenic abscess is 2.86 and in an infiltrate 2.94 [9].
The proteolytic activity of P. buccae (and especially of P. intermedia and P. nigrescens) explains its ability to extend through the cervical planes [4]. Prevotella spp, F. nucleatum and S. anginosus are involved in the pathogenesis of odontogenic abscesses [9]. P. buccae, P. oris, P. intermedia and P. oralis predominate in large abscesses [9].
Prevotella spp has also been isolated in periapical abscesses in non-endodontized and necrotic teeth (P. buccae in 50%, P. nigrescens in 40%, P. tannerae in 20% and other genera in 15%) [3].
In the case presented, the isolation of P. buccae was determinant to establish the dental origin of the infection, as it belongs to group 1 [1].
However, most of the DNI are polymicrobial and the isolated bacteria belong to group 2 and the dental cause can be underestimated, which is why intraoral exploration by a dentist and the review of dental history are necessary to rule out chronic oral pathological processes in patients with DNI [1].
The case presented is an example of DNI with severe progressive symptoms that began with dysphonia and left laryngeal paralysis in which the dental origin was established after the isolation of Prevotella buccae in the culture of the sample obtained from the abscess by cervicotomy and drainage.
It is necessary to systematize the criteria for the diagnosis of DNI including oral examination, dental history, oral radiology and microbiological culture to establish their possible dental origin.
A greater preventive activity on oral pathologies (caries, periodontal disease and oral infectious processes) could reduce the incidence of DNI of dental origin.














