INTRODUCTION
Acute rhinosinusitis often follows an upper respiratory tract infection. It is estimated that only 0.5% to 2% of viral upper respiratory tract infections are complicated by bacterial infection. The prevalence rates for acute rhinosinusitis vary from 6% to 12% [1]. Regarding complications, epidemiological studies estimate an incidence of three complications from rhinosinusitis per million population per year [2].
When the infection involves the frontal sinus, it is defined as acute frontal rhinosinusitis and generally occurs as part of generalized acute rhinosinusitis [3]. Its complications result from progression of the infection outside the sinus, which is relatively rare. Most complications tend to occur in children and young adults because of their thinner sinus walls [3].
Typically, patients with frontal rhinosinusitis come to medical attention with malaise, frontal headache, and tenderness of the orbital margin [4].
The infection usually responds to antibiotherapy. However, it may spread to structures surrounding the sinus [eye, nearby blood vessels, brain, bone, and overlying skin] carrying with them significant morbidity and mortality [5].
Surgical management of frontal sinus pathology remains among the more challenging subjects in otolaryngology and represents one of the most interesting facets of surgical rhinologic practice, requiring a significant level of advanced surgical skills [4].
DESCRIPTION
Case 1
A 40-year-old male patient, with a 1-year history of right-sided frontal pain, presented with a 3-week right ocular pain, swinging pyrexia, and eyelid swelling with erythema. There was no history of trauma, nasal surgery, or paranasal sinus infection.
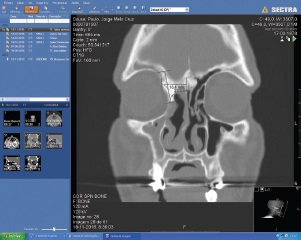
Computed tomography (CT) of the paranasal sinuses revealed a swelling of the eyelid and adjacent preseptal soft tissues, not involving the deeper orbital structures. An extremely dense lesion, with 23 mm cranio-caudal and 18 mm transversal diameters, located in the right frontoethmoidal region was also highlighted, extending to the orbit without invading it (Figure 1).
These findings strongly suggested periorbital cellulitis and was decided to control the infectious process with intravenous antibiotics [ceftriaxone and clindamycin] and dexamethasone for a period of 7 days. After this time and given the fact that the patient still had mild complaints even after a complete course of medical therapy, an external osteoplastic approach combined with endoscopic right frontoethmoidectomy was performed.
The surgical team decided for an external approach to address the frontal segment of the lesion because it allowed for a wide exposure and better control of the whole tumor, which was in direct contact with the superior and medial wall of the orbit.
Perioperatively, from an endoscopic and direct visualization, an ivory-like, smooth, and bony mass was observed, without orbital invasion. Complete resection was achieved.
Case 2
A 18-year-old male patient, without known diseases, presented with a slow growing frontal tumefaction with 1 month of evolution, in association with fever and severe headache. Fluctuant swelling of the frontal region was noticed (Figure 2).
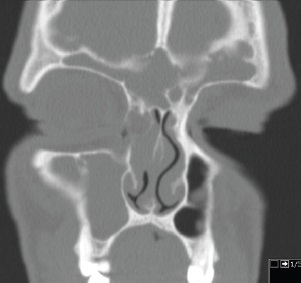
CT demonstrated an anterior table defect of the frontal sinus bilaterally and a left subgaleal abscess and right epidural empyema with focal meningitis. The CT also showed bony destruction of the frontal sinus, indicating osteomyelitis (Figure 3).
Due to a malfunction of the equipment at the time, MRI was not performed, and as it was an urgent surgical patient, the team opted to perform surgery solely with CT support.
The patient was submitted to endoscopic sinus surgery, through a Draf type IIa frontal sinusotomy, and received treatment post-surgically with intravenous antibiotics [ceftazidime, metronidazole and vancomycin] and dexamethasone for 4 weeks.
The results of the cultures revealed the presence of S. aureus spp.
Both patients were free of infection at 2 years of follow-up, without complications.
DISCUSSION
Complications of frontal rhinosinusitis are uncommon but require immediate attention and aggressive treatment to avoid morbidity and mortality [6].
In the first case presented, a frontoethmoidal osteoma gave rise to rhinosinusitis with orbital complications.
Approximately 3% to 4% of the general population have an osteoma in their paranasal sinuses, being the most frequent tumor of the sinonasal tract. These lesions are benign, often found incidentally in the paranasal sinus, more frequently the frontal sinus [80% of cases] [7]. Albeit rarely cause symptoms, these tumors can block sinus outflow when large enough, becoming clinically relevant [4].
About 4% to 10% of all osteomas cause clinical symptoms, which are usually related to the location, size, and growth pattern of the tumor [8].
The most commonly observed symptom is headache, especially located over the area of the osteoma [4]. Likewise, facial deformity, swelling or orbital symptoms are also reported [9].
Osteomas may originate frontal rhinosinusitis that may complicate, giving rise to the development of orbital complications like periorbital cellulitis or periorbital abscess. Patients with intraorbital complications present periorbital edema or erythema, pain, and visual complaints.
Diagnosis of osteoma is usually straightforward on CT, where they appear as rounded, bone-density mass lesions [10]. In the setting of high clinical suspicion of intraorbital and intracranial complications, MRI with and without intravenous contrast is most appropriate, due to its excellent soft-tissue resolution [11]. However, its limited availability and need for sedation in pediatric patients may impair its use. From a practical stand point, the fact that most of these complications are approached in emergency setting [where MRI is often not readily available] makes ceCT the most performed first-line imaging modality by far [12].
Regarding treatment, the general rule is clinical observation for asymptomatic osteomas, surgery is indicated only for large tumors, rapid growth, intracranial or intraorbital extension [6].
Nowadays, even osteomas with lateral extension into the frontal sinus can be removed endoscopically. However, when dealing with large-volume frontal osteomas, like in the first case presented, the need for external access may arise and the osteoplastic flap can be an option. With this technique, wide access to the frontal sinus can be attained. Allowing for radical tumor removal under direct visual control and is indicated in selected patients with orbit and anterior skull base extension [13].
In the second clinical case we presented, the infection extended to the underlying bone and through the skull causing osteomyelitis and focal meningitis complicated with the formation of an abscess.
The prevalence of skull osteomyelitis is 1.5% of all osteomyelitis and it has a mortality rate of 20-40% [14].
This is seen as a complication of acute and chronic frontal rhinosinusitis or trauma and is often associated with other intracranial complications. It is in fact a rare but serious complication, mostly seen in children and adolescents [15].
Due to the high risk of complications, early diagnosis and adequate surgical and antibiotic treatment are required. It is imperative to drain the subperiosteal pus and to establish drainage of the sinus. Presenting symptoms include frontal scalp swelling, headaches, fever, and frontal sinus tenderness [16].
Infection can potentially extend to both intracranial and extracranial spaces to cause periorbital and orbital cellulitis, meningitis, intracranial abscess, and sinus venous thrombosis [4].
While an urgent surgical evacuation of any intracranial complication collection is required, the surgical management of associated rhinosinusitis remains controversial [17].
In our center, we believe that the source of infection must be eradicated since delay in surgical intervention has been associated with prolonged hospitalization. In this patient, we used a Draf Type IIa procedure that consists of widening of the frontal outflow tract with the removal of cells, usually known as “uncapping the egg” technique [4].
In both cases presented, the patients were properly treated with good outcomes, avoiding potentially more dangerous complications.