1. INTRODUCTION
Obesity is an important multifactorial disease that is rising in both children and adults [1]. It is an imperative public health problem affecting approximately 25-30% of children worldwide [2], and studies have shown that 50% of obese adolescents are also obese in their adulthood [3]. Furthermore, adult obesity is associated with the augmented risk of mortality and morbidity [4]. Overweight and obese children have elevated levels of white blood cells, lymphocytes, C-reactive protein (CRP), interleukin 6, and tumor necrosis factor-alpha. There is subclinical systemic inflammation in obesity [5, 6].
Inflammation results from a complex network of interactions involving immune system-related cells such as neutrophils, lymphocytes, monocytes, and macrophages. Clinical studies have shown that the number and proportion of lymphocytes, neutrophils, and other blood cells may reflect the presence and degree of chronic inflammation [7]. Neutrophil/lymphocyte ratio (NLR, neutrophil count/lymphocyte count), platelet/lymphocyte ratio (PLR, platelet count/lymphocyte count), and monocyte/lymphocyte ratio (MLR, monocyte count/lymphocyte count) are indicators that reflect the degree of inflammation and defined as accessible and cost-effective inflammation markers [8, 9, 10]. Studies have reported that inflammatory hematological rates such as NLR, PLR, and MLR are associated with BMI and obesity [11, 12, 13].
Obesity causes an increased risk of cardiovascular morbidity and mortality through different mechanisms such as augmented dyslipidemia, prothrombotic tendency, type 2 diabetes mellitus, and obesity-related hypertension [14]. Changes in lipid profile tests such as an increase in serum total cholesterol, triglyceride, and low-density lipoprotein (LDL-cholesterol) levels and a decrease in high-density lipoprotein (HDL-cholesterol) levels can be observed in obese adolescents [15]. The most common cause of cardiovascular diseases is atherosclerosis accompanied by dyslipidemia and thrombosis [16].
It is known that monocytes play a role in atherosclerosis, and HDL plays a role in the prevention of atherosclerosis and cardiovascular diseases. HDL inhibits the function of monocytes in atherosclerosis and cardiovascular disease [17, 18, 19]. In this context, it has been shown that the monocyte/HDL-cholesterol ratio increases in many diseases, especially in atherosclerosis and cardiovascular diseases, and that the monocyte/HDL-cholesterol ratio can be used as a predictive marker in many diseases [19, 20]. Studies have shown that this rate is associated with obesity and metabolic syndrome [21, 22]. The difference of this ratio from other inflammatory hematological ratios is that; it does not only consist of hematological data but also has a lipid component.
Based on these data, we aimed to examine the changes in inflammatory hematological parameters in obese adolescents and to show the relationship of monocyte/HDL ratio, which is containing a lipid component, with other inflammatory hematological parameters.
2. MATERIALS AND METHODS
Ethics committee approval was obtained for our study with the date 01/07/2021 and the number of 275. After ethics committee approval, we retrospectively analyzed the files of 60 patients, 30 obese and 30 healthy controls, aged 11 to 16 years, who applied to the pediatric outpatient clinic between January and May 2021. We evaluated adolescents with a body mass index (BMI) of 95% and above as obese adolescents [23]. HOMA-IR was calculated with the formula (insulin IU/L x glucose mg/dL)/405 for the determination of insulin resistance. Laboratory tests, hematological parameters, gender, age, and BMI were compared between the groups. Correlations between monocyte/HDL-cholesterol and other parameters were examined in the obese group.
Blood was taken into tubes containing ethylenediamine tetra-acetic acid (EDTA) as an anticoagulant for hemogram, and into tubes with non-anticoagulant gel for biochemistry parameters.
2.1. MEASUREMENT OF HEMATOLOGICAL PARAMETERS
Red blood cells, white blood cells, neutrophils, monocytes, lymphocytes, and platelets were evaluated in complete blood count. Blood tests were performed on Mindray BC 6800 (Mindray Building, China) with their original kit. The BC 6800 hematology analyzer used sheath flow impedance, laser scatter, and SF Cube analysis technology. NLR was obtained by dividing the neutrophil count by the lymphocyte number, PLR by dividing the platelet count by the lymphocyte count, MLR by dividing the monocyte count by the lymphocyte count, and monocytes/HDL-cholesterol by dividing the monocyte count by the HDL-cholesterol level.
2.2. MEASUREMENT OF OTHER LABORATORY TESTS
Glucose, urea, creatinine, aspartate aminotransferase (AST), alanine aminotransferase (ALT), CRP, total cholesterol, triglyceride, HDL-cholesterol, and LDL-cholesterol tests were measured with colorimetric method; thyroid-stimulating hormone (TSH) and insulin tests were measured in the an auto-analyzer (Roche Brand, Cobas 8000 model, USA) by chemiluminescence immunoassay method. HbA1c was measured by the high-performance liquid chromatography method in auto-analyzer (Biorad, Variant II turbo, Japan). LDL-cholesterol was calculated using the Friedewald formula [LDL-cholesterol = total cholesterol - (HDL-cholesterol) - (TG/5)].
2.3. STATISTICAL ANALYSIS
The suitability of the parameters to the normal distribution was evaluated by Kolmogorov-Smirnov and ShapiroWilks tests. The student's t-test was performed for the comparison of normally distributed parameters between two groups, and the Mann Whitney U test was applied for the comparisons between two groups of parameters that did not show normal distribution. Pearson correlation analysis was performed to examine the relationships between parameters conforming to the normal distribution, and Spearman'srho correlation analysis was used to examine the relationships between parameters not conforming to the normal distribution. Continuity (Yates) Correction was performed to compare qualitative data. Significance was evaluated at the p<0.05 level.
3. RESULTS
The study was conducted with a total of 60 adolescents aged between 11 and 16 years. Adolescents were evaluated under two groups as “Obese” (n=30) and “Control” (n=30). There was no statistically significant difference between the groups in terms of mean age and gender distribution (p>0.05).
BMI, ALT, CRP, triglyceride, insulin, and HOMA-IR levels of obese children were statistically significantly higher than the control group (p<0.05). There was no statistically significant difference between the obese and control groups in terms of other study parameters (p>0.05) (Table 1).
Table 1: Evaluation of the groups in terms of study parameters.
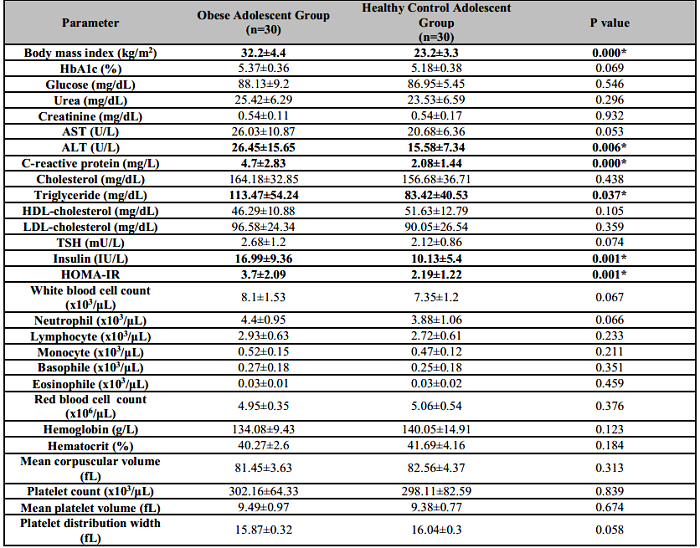
Results are expressed as mean±standard deviation.
*p<0.05.
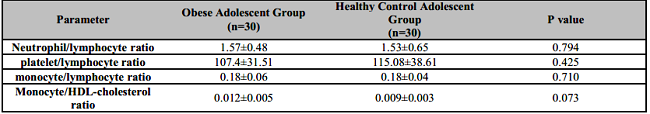
There was no statistically significant difference between the obese and control groups in terms of inflammatory hematological rates (p>0.05) (Table 2).
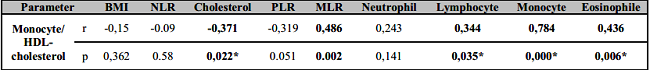
In the obese group, there was a positive, moderate (48.6%), and statistically significant relationship between monocyte/HDL-cholesterol and MLR (p<0.05). There was a positive, moderate (45.6%) and statistically significant correlation between monocyte/HDL ratio and WBC and eosinophil counts (p<0.05). There was no statistically significant relationship between monocyte/HDL ratio and other study parameters (p>0.05) (Table 3).
4. DISCUSSION
Childhood obesity is associated with chronic inflammation and is an important cause of cardiovascular risk. New biomarkers associated with subclinical inflammation such as NLR [12], PLR [13], MLR [11], and Monocyte/HDL-cholesterol [21, 22] have been investigated in obesity, before. These parameters or indices are derived from calculations formulated from the results of routine blood analysis. However, the monocyte/HDL-cholesterol ratio comprises a lipid component. In this study, we examined inflammatory hematological ratios such as NLR, PLR, MLR, and monocytes/HDL-cholesterol, as well as hemogram parameters, in adolescent obesity. We found that the NLR, PLR, MLR, and monocyte/HDL-cholesterol values of the obese adolescent group were not different from the control group. Our findings did not support the utility of inflammatory hematological rates as a biomarker in adolescent obesity.
In obese individuals, inflammatory cells infiltrate into adipose tissue and produce cytokines in adipocytes together with these cells, causing low-level chronic systemic inflammation [24]. In recent years, rates such as NLR and PLR, which are accepted as indicators of subclinical inflammation, have been investigated in obesity and obesity-related diseases [5, 12, 25]. However, investigations about these rates in pediatric and adolescent obese groups are limited.
Aydın et al. [12] reported higher NLR in obese adolescents than in the control group. Santoz et al. [13] reported a positive correlation between NLR and BMI in their study on obese children. Dilek et al [26] did not find any difference in NLR in obese adolescents compared to the control group. Similar results were obtained in another study in obese patients and they emphasized that NLR is not a good marker of inflammation [5]. Similarly, we did not determine any difference in NLR levels. Based on these data, the utility of NLR as an inflammation marker in obese adolescents is controversial.
Platelets are involved in coagulation. In addition, by secreting proinflammatory cytokines, they cause leukocyte migration and attachment to the endothelial cells and thus play an important role in inflammation [13]. Increased values of PLR are associated with cardiovascular diseases and conditions that increase the risk of cardiovascular disease [27]. When we examined the studies in obese adolescents, Aydın et al. [12] and Dilek et al. [26] reported that PLR was not different in obese adolescents compared to healthy controls. Again, Santoz et al. [13] found no correlation between NLR and BMI in their study on obese children. We obtained similar results in our study. Therefore, we believe that PLR value cannot be suggested as an inflammation marker in obese adolescents.
MLR is considered a new, inexpensive and reproducible marker suitable for routine use in determining the systemic inflammatory response and can be calculated from a hemogram test and under simple laboratory conditions. In a study, MLR was found to be an independent risk factor for the presence of cardiovascular diseases (CVD) and was associated with the lesion severity in patients with previous coronary artery disease [28]. In another study, it was reported that MLR is a strong and independent predictor of CVD mortality [29]. Mete et al [11] did not find any correlation between MLR and BMI in obese and overweight patients. In our study, we found similar MLR values in the obese and control groups. Therefore, we believe that MLR value cannot be used as an inflammation marker in obese adolescents.
Monocytes make up roughly 3-8% of circulating leukocytes and, along with other cells, are essential components of the innate immune system. In tissues, circulating monocytes and their differentiated forms, known as macrophages, play central roles in the initiation and resolution of inflammation; this is mainly through phagocytosis, the release of inflammatory cytokines, presence of reactive oxygen species, and activation of the adaptive immune system [30]. Excessive activation of monocytes exacerbates atherosclerosis and immune diseases, leading to the activation of platelets, endothelial cells, and prothrombotic pathways [31]. HDL neutralizes the pro-inflammatory and pro-oxidant effects of monocytes by inhibiting the oxidation of LDL molecules and the migration of macrophages, as well as promoting cholesterol efflux from these cells [32].
It has been reported that the monocyte/HDL-cholesterol ratio, which is accepted as an inflammatory marker, is a new and prognostic indicator of mortality and morbidity in many diseases [33]. It has been reported that the change in the monocyte/HDL-cholesterol ratio is associated with cardiovascular diseases [34], obesity, and metabolic syndrome [21, 22]. However, studies in obese subjects are limited. Usta et al. [22] and Vahit et al. [35] showed that the monocyte/HDL-cholesterol ratio is a marker of the metabolic syndrome characterized by obesity, increased serum glucose levels, increased blood pressure, increased LDL-cholesterol, and decreased HDL-cholesterol levels. We, on the other hand, found that the monocyte/HDL-cholesterol ratio in obese adolescents was not different compared to healthy controls. In line with our data, it is difficult to use the monocyte/HDL-cholesterol ratio as an inflammation marker in obese adolescents.
In addition, in our study, we found an inverse relationship between the monocyte/HDL-cholesterol ratio and MLR in obese adolescents. Variables that make up the difference here are HDL-cholesterol level and lymphocyte count. In our study, we did not find a statistically significant difference in HDL-cholesterol and lymphocyte counts in the obese group, however, HDL-cholesterol was lower and lymphocyte count was higher in the obese group. Decreased HDL-cholesterol level is a part of dyslipidemia seen in obese individuals [15]. In addition, increased T lymphocyte count has been reported in obese patients and it has been reported that this is associated with increased cytokine levels in obese patients [36]. In this way, HDL-cholesterol and lymphocyte counts, which vary in different directions in obese patients, explain the inverse relationship between monocyte/HDL-cholesterol and MLR in our study. However, further investigations are warranted to elucidate this relationship. In addition, we did not detect a correlation between monocyte/HDL-cholesterol ratio and NLR, PLR, or CRP levels.
Several limitations should be taken into account in our study. The cross-sectional design of our study does not allow exploring causality and temporal relationship between the studied variables. The sample size of our study is among the limitations of our study. Inflammatory cytokines were not evaluated in our study which is another limitation. Therefore, studies with larger samples are needed, including inflammatory processes.
5. CONCLUSIONS
In our study, the NLR, PLR, MLR, and monocyte/HDL-cholesterol values of the obese adolescent group were similar to the values of the control group. There was an inverse correlation between monocyte/HDL-cholesterol and monocyte/lymphocyte ratios. There was no correlation between monocyte/HDL-cholesterol ratio and other rates. Our data do not support the utility of inflammatory hematological rates as a biomarker in adolescent obesity. Although studies with larger sample sizes are warranted on this subject, we believe that our results can shed light on other studies to be conducted.