INTRODUCTION
Advances in the field of medicine have caused an increase in the geriatric age group in the world [1]. Although advanced age is not assumed as a disease, physiological changes in this group of patients make them more susceptible to both surgical and medical conditions [2].
Geriatric syndromes include cognitive impairment, delirium, depression, fecal incontinence, mobility decline and urinary incontinence (UI) are associated with significant morbidity [3]. These syndromes, which are quite common, have multifactorial etiological causes [3, 4]. Multiple drug use, malnutrition and pain are some important etiological factors in this age group [3]. UI is the most common of these syndromes [5]. UI is an important cause of poor quality of life (QoL), morbidity and mortality in geriatric patients [5].
Age, gender, number of births, previous urogenital surgery, obesity and chronic disease are reported risk factors for UI [6]. In addition, mental problems such as cognitive impairment are also related to UI [3, 6]. Among older adults, UI is more likely to occur not only because of underlying diseases, but also because of the various functional disabilities that patients have at the time of hospital admission [6].
There is a lack of specific research in geriatric patients of UI and UI-related QoL in a surgical clinic [7]. Moreover, there is not enough information about incontinence in men, as most studies have focused on women [3].
The aim of this exploratory study were to examine the effect and coexistence of geriatric syndromes, admission type and surgical severity on UI-related QoL in patients hospitalized in the urology clinic.
MATERIAL AND METHODS
Geriatric patients (65 and over years old) who were hospitalized for various reasons and for more than 3 days between October 2019 and March 2020 were prospectively evaluated at Zonguldak Bulent Ecevit University department of Urology, Zonguldak, Turkey. Patients who were hospitalized for less than three days, transferred to another clinic, had severe dementia findings (severe cognitive decline), severely impaired general condition, illiterate, advanced vision and hearing problems and refused to participate in the study were excluded from the study. The patients were grouped according to the type of hospitalization (emergent and non-emergent) and surgical weight. Continence status and related quality of life of the patients were questioned. We also examined geriatric syndromes and some of their known associated risk factors. Approval was obtained from the local ethics committee of Zonguldak Bülent Ecevit University (protocol number: 2019-47-03/04), and before participating in the study, written consent was obtained from the patient or their relatives according to patients’ level of cognitive status.
All measurements were made face-to-face and by trained personnel, using standardized questionnaires.
DEMOGRAPHY AND COMORBIDITIES
Demographic data such as age, gender, marital status, educational status, body mass index, comorbidity, number of drugs used, American Society of Anesthesiologists (ASA) scores, surgical data and length of hospital stay were recorded. The patient was questioned and the surgical history and data such as hypertension, diabetes mellitus and cerebrovascular disease were obtained.
-
Urinary incontinence:
ICIQ-SF complemented by patients with UI to assess the severity as well as its effect on QoL. This questionnaire consists of four subscales. The total score consists of the sum of points of the first three questions. According to this score, the severity of UI is divided into 5 groups. We evaluated the QoL in relation to the UI using the third question of ICIQ-SF.
-
Geriatric syndromes and related factors:
The patients were evaluated using various validated questionnaires in terms of the presence of geriatric syndrome as well as polypharmacy, mulnutrition, pain and fecal incontinence that may be associated with UI. Cognitive impairment, delirium, depression, and decreased mobility were considered the main geriatric syndromes.
Cognitive function was assessed using a standardized Mini Mental State Examination (MMSE) Test [8]. Scores of 25 and above are considered normal. A score of less than 13 indicates a serious cognitive decline. Scores between 14-20 indicate moderate and scores between 21-24 indicate mild cognitive decline. The Geriatric Depression Scale Short Form consisting of 15 questions was used to evaluate the presence of depression. 8 points and above was accepted as depression. Delirium was screened using the Nursing Delirium Screening Scale consisting of 5 questions. If the score was greater than 2, the presence of delirium was accepted. Malnutrition was assessed using the Malnutrition Screening Test. Patients having a score more than 2 points were considered to have malnutrition. Intestinal functions of the patients were evaluated using the Low Anterior Resection Syndrome (LARS) score form. The presence of fecal incontinence was accepted in patients with a total score of 2 and above.
''Can you climb the stairs without help?" and "Have you had more than a day of pain in the past 2 weeks?" were the questions to affirm the existence of mobility decline and pain. "How many drugs are you currently taking?" was the question to affirm polypharmasy defined as having more than 5 drugs [9].
SURGICAL HISTORY
Elective hospitalisation was assumed when patients admitted to the hospital according to the elective appointment list; for patients admitted from the emergency department or outpatient clinic or transferred from another center on an unplanned basis non-elective hospitalisation was assumed.
Looking at the literature, there is no standard definition for surgical weight [10]. The concept of major and minor surgery is still being discussed. It is generally recommended to define minor surgery for surgeries that can be performed in office conditions; it has been suggested to define major as a minor procedure that may pose a risk to the patient. In this framework, surgeries (open surgeries and percutaneous surgeries) that must be performed in an absolute hospital environment are defined as major surgery. Minimally invasive endoscopic procedures were defined as minimal, and minor procedures were also considered major, considering the patient's comorbidity and condition during the procedure [10]
STATISTICAL ANALYSIS
The conformity of univariate data to normal distribution was evaluated with the Shapiro-Wilk test. Mann-Whitney U test was used together with Monte Carlo results to compare two independent groups with each other according to quantitative data. In the comparison of more than two groups according to quantitative data, Jonckheere-Terpstra Test and Kruskal-Wallis H Tests were used together with Monte Carlo results, while Dunn's Test was used for Post Hoc analyses. Spearman's rho test was used to examine the correlations of the variables with each other. In comparison of categorical variables with each other, Pearson Chi-Square and Fisher Exact and Fisher-Freeman-Halton tests were tested with Monte Carlo Simulation technique and column ratios were compared with each other and expressed according to Benjamini-Hochberg corrected p value results. Logistic regression test was used to determine the cause - effect relationship of the incontinent state with other explanatory variables, first one by one (Enter) for each variable, and then the model using the Backward screening method for both conditions with and without correcting the important variables according to age, gender and length of hospital stay created. Quantitative variables were expressed as Median (Percentile 25 / Percentile 75) in the tables, while categorical variables were shown as n (%). Variables were analysed at a 95% confidence level and a p value of less than 0.05 was considered significant. SPSS 26.0 (IBM Corporation, Armonk, New York, United States) program was used in the analysis of variables.
RESULTS
Among 250 patients, 140 reported experiencing UI in the previous 4 weeks though no statistically significant difference was seen between genders (p=0.073). Mean age of patients was 72.9±5.9 (min: 65-max: 90) years. Of the patients 190 (76%) were male and the median length of stay was 6 days (interquartile range 4-11 days). Patients’ sociodemographic characteristics are summarized in Table 1. 82.4% of the participants had a urological operation, 17.6% of them were hospitalised to treat conservatively. While the majority of the admissions were elective (90.8%), only 20.8% of the patients underwent a major surgery.
Table 1. Patient's baseline sociodemographic characteristics
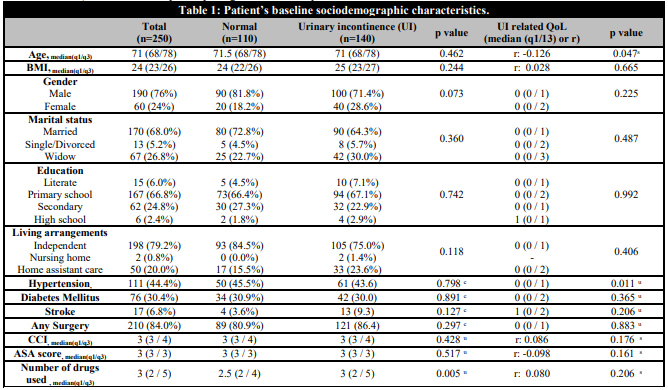
BMI: Body mass index; CCI; Charlson comorbidity index; ASA: American Society of Anaesthesiologists.
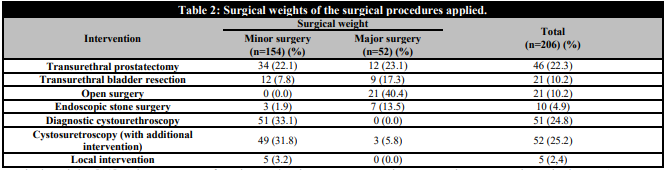
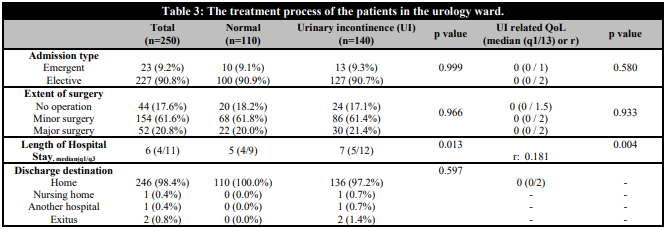
The surgical weights of the surgical procedures we applied to our patients and the treatment process of the patients are summarized in Table 2 and Table 3.
All patients had at least one geriatric syndrome. The relationship of UI with geriatric syndromes and related factors are shown in Table 4. Nothing but cognitive impairment appears to be associated with UI among geriatric syndromes (p=0.007). When evaluated in terms of the level of cognitive impairment, it is seen that there is no significant difference in mild impairment symptoms of the patients, but moderate impairment findings are more common in patients with impaired continence (p=0.005). Among the UI-associated conditions, patients with incontinence seem to use more medication (p=0.005).
Table 4. The relationship of urinary incontinence (UI) with geriatric syndromes and related factors
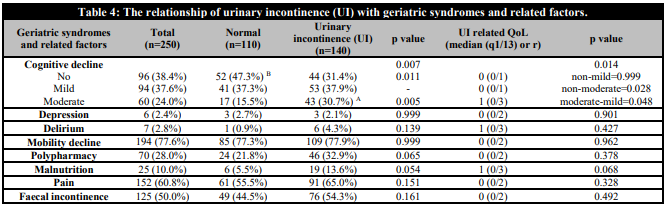
A Expresses significance relative to the non-incontinence group; B Expresses significance according to the group with incontinence.
When UI-related QoL was evaluated, it is seen that there is only a statistically significant relationship between cognitive impairment among geriatric syndromes (p=0.014). There is an inverse correlation between the cognitive impairment level of the patients and their QoL. There is a statistically significant relationship with UI-related QoL, inversely proportional to the length of stay in acute ward and directly proportional to their age (p=0.047, p=0.004, respectively).
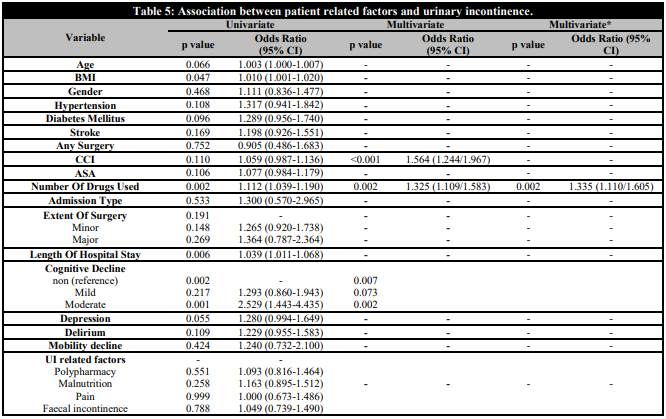
In the multivariate analysis (Table 5), it is seen that moderate cognitive decline increases the possibility of UI more than 3 times and this increase continues when adjusted according to the age, gender and length of stay in acute ward. Charlson Comorbidity Index (CCI) (odds ratio [OR], 1.56; 95% confidence interval [CI], 1.24–5.05) and the number of medication used (odds ratio [OR], 1,33; 95% confidence interval [CI], 1.11–1.58) were also associated with increased probability of having UI.
DISCUSSION
In the elderly population, the patient because of embarrassment and consideration as a natural consequence of aging rarely reports UI [11]. Often, affected individuals reject and hide the presence of UI, causing physical and psychosocial restrictions to enjoy life. It is associated with poor QoL, which includes loss of self-confidence and social isolation in addition to negative consequences such as anxiety, depression, impaired sexual life and decreased physical activity [12, 13].
In this study, we revealed the factors affecting UI-related QoLin the elderly patient population hospitalised in the urology ward. Although UI can be seen in both genders, in general, the prevalence of UI in women is reported to be twice more than in men [7, 14]. This difference is generally tried to be explained by anatomical differences. Even we observed UI to be higher in women than in men in our study, this difference was not statistically significant. In a German aging survey conducted by Buczak-Stec, it was reported that the quality of life was more affected in men [15]. In a meta-analysis by Kwon et al., it was reported that women's UI-related QoL was worse [16]. In the other meta-analysis performed by overcoming the small sample size, no gender difference was observed [17]. Similar to this study, we did not find a gender relationship in terms of UI-related QoL. Therefore, in our study, UI seems to affect the QoL equally in both genders. Patients with and without UI were similar in terms of age groups. When we look at the UI-related QoL, it is seen that there is an inverse relationship with age. We think this is a momentous finding. As, the term QoL includes various domains in human life that describes the expectations of an individual or society for a good life [7], this issue may be a consequence of decreased expectations or a result of shame of patients. This is in line with the findings of Pizzol et al. [7] However, Alappattu et al.’s study, in which patients with various neuromuscular diseases were evaluated, revealed the contrary [18].
The severity of cognitive impairment and the degree of inactivity are the two most important determinants of incontinence in dementia patients [19]. In our study, we found a significant relationship between cognitive impairment and UI. Moreover, in the regression analysis, we found that while mild cognitive impairment was not a risk factor for UI, moderate cognitive impairment increased the risk of UI more than 3 times, regardless of age and gender. Problems in mobilization have been shown to be more important predictors of incontinence than the severity of dementia. [19]. Although this finding is consistent with the current literature [17, 19], we could not reach a similar conclusion between mobility restriction and incontinence in our patients. Moreover, we found that as the cognitive functions deteriorated, the QoL scores expressed by the patients also worsened. We think that this situation can be explained by the enhancing effect of cognitive impairment and UI in patients. Although the presence of depression and delirium are geriatric syndromes that impair QoL, we could not find a relationship between patients' QoL associated with UI.
Polypharmacy is known as a risk factor for UI [3]. In our study, the number of drugs used by UI patients, regardless of age and gender, was statistically significantly higher. However, when we defined it as polypharmacy, we could not see a statistical significance among the patients. In addition, we could not find a relationship between the amount of medication used and the patients' QoL. When we look at the literature, we see that there is no standard terminology in the definition of polypharmacy [20]. We think that this inconsistency in our study may be related to the lack of definition in this standard.
The relationship with UI and increased comorbidity of the patients is known [6]. The risk increases with both the effect of the current disease and the effect of the drugs used for these diseases. In our study, we could not find a significant relationship between patients' existing systemic diseases such as hypertension, diabetes mellitus and stroke and UI. Although there was not a significant difference between groups when we used CCI, we saw a risk relationship between CCI and UI in the regression analysis. A recent meta-analysis aimed at finding the relationship between patients' comorbidities and UI-related QoL failed to show this relationship [7]. Similar to the literature, in our study, we could not find a relationship between comorbidities and UI-related QoL.
When we searched the literature, we could not find any study examining the relationship between the type of hospitalization and the UI associated QoL. In the study of McRae et al. reported that non-elective hospitalizations increased the risk of developing geriatric syndromes [21]. In the same study, the likelihood of geriatric syndrome increases as the severity of surgery increases [21]. Although the concept of our study was different, we could not find a relationship between UI and the way patients applied to the hospital. Similarly, there were no relationship between the type of hospitalization and the patients' UI associated QoL. In addition, we could not find a relationship between surgical severity and UI and UI-related quality of life.
Our aim was to address the UI-related QoL of cross- sectional geriatric patients. However, it would be better to evaluate our study with its limitations. We think that the fact that we accept UI as the presence of uncontrolled urine flow in our study may be a factor that prevents us from making an adequate interpretation. Designing the study according to UI subtypes will enable us to reach a precise conclusion. All of our patients had at least one geriatric syndrome, which actually seemed very high. In addition, since our evaluations were instantaneous, we could not distinguish whether we were evaluating the existing complaints of the patients or the newly developed situation. Additionally, the fact that the definition of polypharmacy is not standardized may affect the results of the study. Therefore, we think that this problem can be overcome by designing a multicentre study with a large number of patients using definitions that are more standard.
Despite these limitations, our findings in this cross-sectional study that we conducted in our urology clinic are valuable. The geriatric age group constitutes a significant portion of the patients admitted to the urology clinic. Most of these patients have at least one geriatric syndrome and comorbidities that may predispose to it. UI has an important place in urology practice and it further reduces the quality of life of patients who already have low quality of life.
In conclusion, this study highlights the necessity of supporting elderly incontinence patients with geriatric syndrome followed in the urology clinic. In particular, evaluating and supporting their cognitive functions, reviewing and regulating the drugs they used will contribute significantly to the QoL in this patient group.