1. INTRODUCTION
Mucocele, also known as the mucous retention phenomenon has the most common occurrence in lower lip [1, 2]. It can also occur in the paranasal sinus, known as sinus mucocele, which most commonly involves the fronto-ethmoid sinus followed by the maxillary sinus (2.7-10%) [2, 3, 4].
Mucocele develops in the maxillary sinus due to obstruction of the drainage ostium, because of chronic sinusitis, polyps, bone tumours, trauma, or after surgery [5]. Presentation depends on the extent of expansion within the sinus and the involvement of adjacent structures [2]. Assessment of the extent is made through conventional radiographs such as water's view and higher imaging techniques such as Computed tomography [1]. Management is surgical removal and if left untreated, it can expand and lead to complications due to nasal and orbital involvement.
Many theories have been suggested to explain the mechanisms responsible for the formation and growth of mucoceles, including cystic degeneration of a seromucous gland, even though the histopathological and molecular examinations showed a dynamic process of bone resorption, where inflammation takes part, through cytokines, which act between the bone and the epithelium releasing prostaglandins [6, 7]. These play a key role in the development of a mucocele, along with the sinus obstruction. Mucoceles, in turn, can be caused by a facial trauma or previous surgery which could result in compartmentalized areas [6, 7].
Here, we report a case of mucocele in the maxillary sinus in a 20-year-old male along with its clinical presentation, radiological and histopathological findings, and surgical management with follow-up.
2. CASE REPORT
A 20-year-old male patient reported to the Department of Oral Medicine and Radiology of a Tertiary Care Dental Hospital with the chief complaint of swelling in his left cheek region for 8 months. According to the patient, the swelling was initially small, insidious in onset, and gradually progressed to its present size. There was an associated history of trauma 2 years ago. No specific surgical treatment was performed after the trauma. There was no history of fever, pain or pus discharge associated with the swelling. No history of extraction of the tooth or any recent dental treatment. There was no history of nasal obstruction, cold, allergic rhinitis, and acute or chronic sinusitis.
On Extraoral examination, a diffuse swelling was present on the left side of the face extending superiorly up to the left infraorbital region, inferiorly up to the region of the upper lip, medially up to the lateral border of the nose, and laterally approximately 4 cm in front of the left tragus of ear (Figure 1A). On palpation, the swelling was non-tender and firm to hard in consistency.
Intraorally, there was evidence of buccal & palatal expansion with obliteration of buccal vestibule with respect to 25, 26, and 27 (Figure 1B). On palpation, it was non-tender, soft to firm in consistency, and compressible. Orthopantomograph (OPG) revealed a large expansile radiolucent lesion with well-defined non-continuous corticated borders extending from 25 to 27 region and the floor of the maxillary sinus was not visible (Figure 1C). Contrast-enhanced computed tomography (CECT) scan revealed, a large unilocular lytic lesion causing expansion of the superior alveolar arch of the left maxilla accompanied by thinning of adjacent cortices. The lesion was seen in relation to the left upper premolar and in relation to the roots of first molar, with evidence of root resorption of the same and displacement of the adjacent molar tooth. Superiorly, the lesion is protruding into the maxillary sinus causing its near complete obliteration and opacification. Superomedially, it is also projecting into nasal cavity causing its narrowing, inferomedially it is projecting into oral cavity, & laterally projects into vestibule (Figure 1D, E). The features were suggestive of a maxillary mucocele.
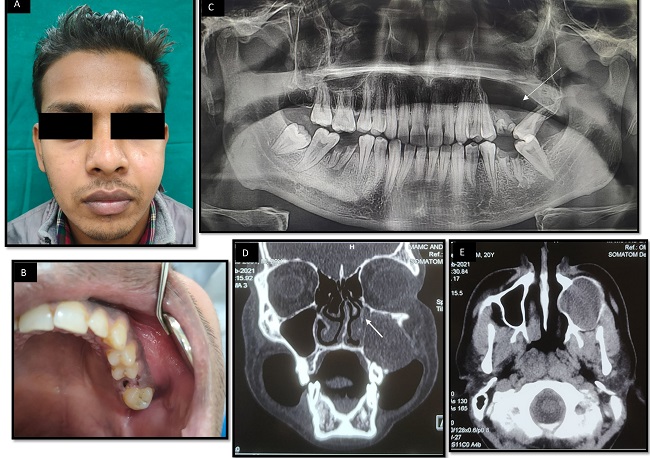
Figure 1: A: Extraoral Photograph showing gross facial asymmetry on left side of face. B: Intraoral photograph showing root stump of 26 with buccal and palatal expansion. C: OPG showing large radiolucent lesion extending from 25 to 27 with loss of floor of left maxillary sinus and displacement of 27. D: Coronal section hard tissue window showing complete opacification of left maxillary sinus and extending medially into nasal cavity (Arrow). E: Axial section soft tissue window showing complete opacification and expansion of left maxillary sinus.
The case was further planned for incisional biopsy under local anaesthesia. Histopathological examination revealed a cystic wall lined by continuous ciliated pseudostratified columnar epithelium. Few areas were showing discontinuous non-keratinized stratified squamous epithelium of 1-2 cell layer thickness, which was continuous with antral lining. Numerous goblet cells and mucus cells were noted in the epithelial lining (Figure 2A and 2B). Excision of the cyst was planned for the patient. An ostectomy was performed using rotary instruments to enlarge the bony cavity. The distinct soft tissue lining was separated from the maxillary sinus lining and excised using curettes (Figure 2C). Sharp margins were rounded off with rotary instruments. Primary closure with 3-0 vicryl suture was achieved. The gross specimen (Figure 2D) was sent for histopathological examination which was consistent with the diagnosis Mucocele of Maxillary Antrum.

Figure 2: A: Incisional (HE x 10X) as well as B. B: excisional biopsy (HE x 40X) showed presence of cystic lumen lined by pseudostratified ciliated columnar epithelium continuing into discontinuous nonkeratinized epithelium. Some areas showed presence of goblet cells and mucous cells. C: Surgical exposure of the lesion via Caldwell-Luc approach. D: Gross Pathologic specimen.
After 2 weeks of post-operative follow up, there was evidence of uneventful healing at the surgical site (Figure 3A, B, C). After 3 months of follow up, OPG revealed good bone fill at the operated site (Figure 3D, E, F).
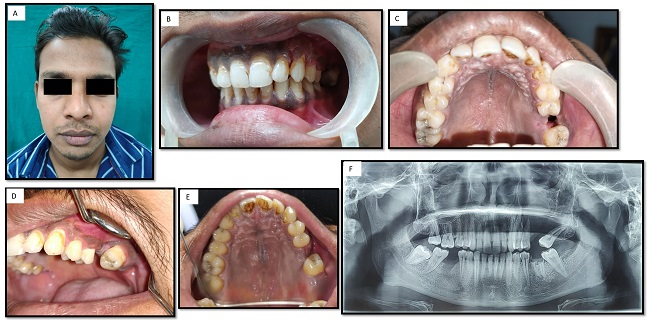
Figure 3: 2 weeks post-operative. A: Extraoral photograph showing facial symmetry. B and C: Intraoral photograph showing healed surgical site. 3 months post-operative D and E: Intraoral photograph with evidence of complete healing. F: Orthopantomograph showing evidence of bone fill at surgical site.
3. DISCUSSION
Mucocele of the maxillary sinus falls under retention type, caused due to obstruction of the sinus ostium, resulting in impaired drainage and accumulation of mucus in mucoperiosteal-lined cavity [3]. The common etiology for maxillary sinus mucoceles is believed to be untreated trauma, history of prior sinus surgery, facial fractures, and with no cause in some cases. It is considered to result from entrapped sinus mucosa, removal of the sinus mucosa in chronic sinusitis, and secondary to cicatricial bridles from previous surgeries [3]. All these etiological factors finally result in obstruction of the maxillary sinus ostium blocking the drainage of normal sinus secretion, resulting in the accumulation of mucus. It results in gradual expansion of sinus, and eventually thinning and destruction of the bony wall.
Mucocele develops gradually, and has a higher incidence between the third and fourth decade of life, with no reported sex predilection [8]. In maxillary mucocele, there may be bulging of cheek outwards with infra-orbital anaesthesia [2, 9]. Medial extension into the nasal cavity results in nasal obstruction. Inferior extension into the palatal and alveolar bone can cause palatal swelling and mobility of teeth [10]. Superior extension into inferior orbital cavity results in displacement of orbital content, resulting in proptosis, ophthalmoplegia and in vision changes, such as decreased visual acuity, blurred vision, diplopia [1].
The radiographic assessment with Waters views shows enlargement of the sinus cavity and thinning of the bony walls, and the sinus may appear more radiopaque. Computed Tomography (CT) is one of the valuable radiographic tools in diagnosis of maxillary sinus mucocele. Mucocele appears as an isodense homogenous lesion with smooth well-defined margins of bone erosions in sinus walls with displacement of soft tissue structures in CT [2].
The management of maxillary sinus mucoceles is surgical. The traditional method of treatment includes Caldwell-Luc sinusectomy, inferior nasoantral window and mucocele lining removal [4, 5]. It results in postoperative complications such as hypoesthesia or paraesthesia of cheek and lips, and prolonged oedema of buccal region [10, 11]. It is replaced by a recent innovation, the endoscopic sinus surgery, which has very low recurrence rate at or close to 0% with a shorter postoperative recovery and less morbidity [1, 4]. Postoperative regular endoscopic examination and saline irrigation are important methods to prevent recurrence [11].
4. CONCLUSIONS
The misdiagnosis of maxillary sinus mucocele is attributed to uncertain etiology and rare occurrence of mucocele. The case presented here was initially misdiagnosed to be cyst of odontogenic origin. A biopsy is required in such cases to establish true diagnosis. Radiographs play a vital role in replicating the original pathology ongoing within bone and soft tissues, preoperatively.














