The parents of a 3-month-old Caucasian male baby consulted because, since the third week of life, he has presented a reddish-brown lesion on the back of the proximal phalanx of the third finger of the left hand. Since then, the lesion has slowly grown and has recently blistered, leaving a scab. In previous consultations in other centers, he has been diagnosed with an insect bite or burn. The infant was healthy, breastfeeding, was not taking any medication, and had no relevant personal or family history. Since he was born, he has had the habit of sucking the second and third fingers of his left hand. On examination, there was a dry oval scab measuring 4x3 mm. Upon removal, an oval, yellow-brown indurated papule with hemorrhagic residue was observed (Figure 1A). Once the skin had regenerated, the area of the lesion was rubbed and the appearance of intense erythema and the formation of a tense 5x4 mm blister (Darier sign) was observed (Figure 1B). The remainder of the mucocutaneous examination, systemic assessment, and baseline laboratory investigation were normal. Given the clinical suspicion of solitary mastocytoma (SM), a diagnostic excisional biopsy was planned. Surgical excision and follow-up after were uneventful. The histopathological pattern consisted in a dense infiltrate of round cells, resembling mast cells, in the upper third of the dermis, dermo-epidermal junction, and at times in the epidermis (Figure 1C). Immunohistochemical study for c-KIT expression showed that the inflammatory cellularity was mainly CD117 positive, showing the presence of abundant mast cells in the lesion (Figure 1D), which confirmed the diagnosis of SM.
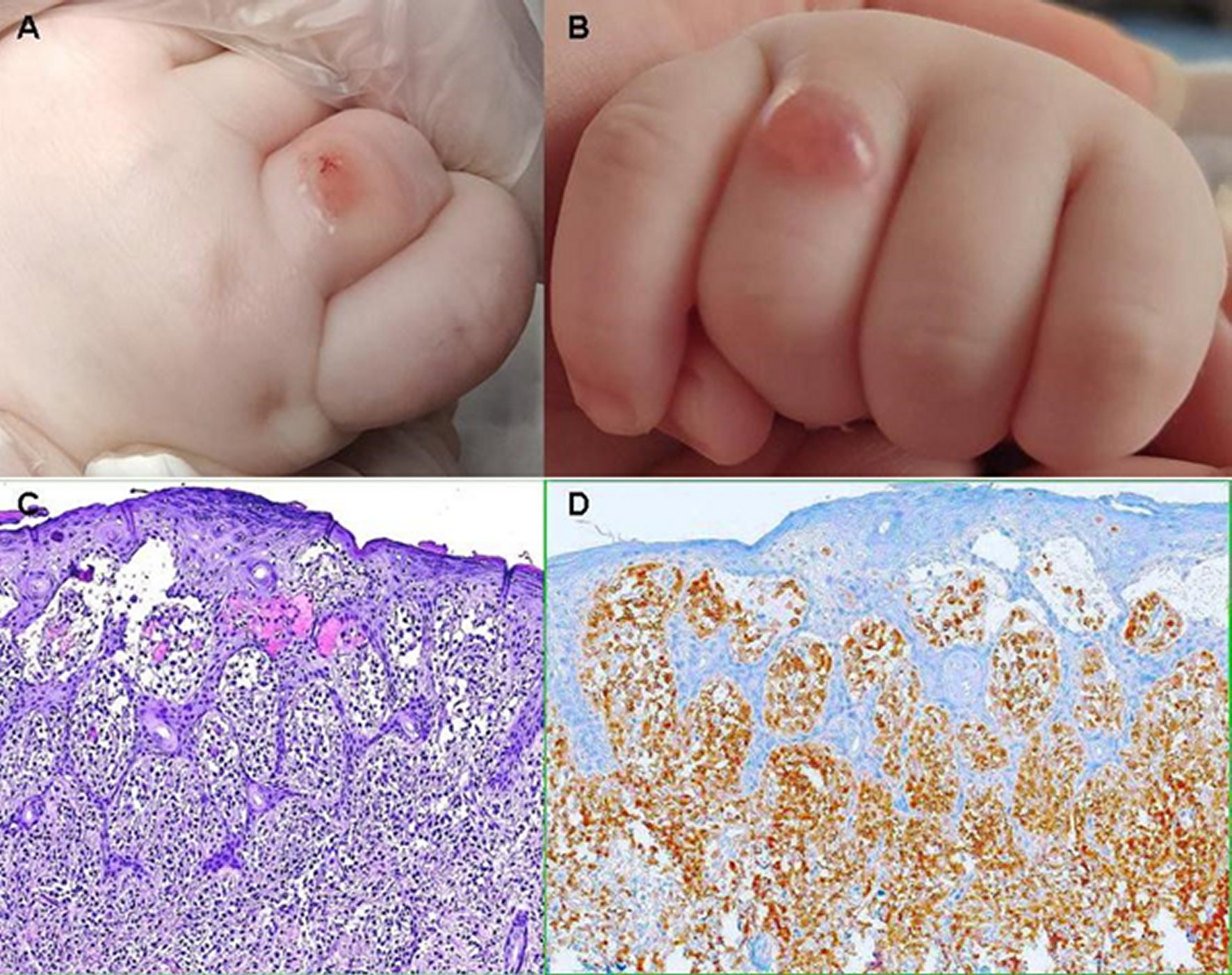
Figure 1 A) Solitary mastocytoma in a 3-month-old infant. B) Rubbing-induced tense blister containing clear liquid (Darier sign). C) Histopathological pattern: dense infiltrate of mast cells in the upper third of the dermis, dermo-epidermal junction, and at times in the epidermis (H&E, ×200). D) An immunohistochemical stain directed against CD117 highlights the mast cell infiltrate (c-KIT, x200).
Mastocytosis is a heterogeneous group of rare diseases, with varying manifestations, characterized by clonal proliferation of mast cells in various organs. Activating c-KIT proto-oncogene mutations have been related to the etiopathophysiology. The c-KIT proto-oncogene, located on chromosome 4q12, encodes KIT (the receptor for stem cell factor, also called CD117), a transmembrane protein that binds to stem cell factor and promotes cell division [1]. The skin is the most frequently affected organ. The World Health Organization classifies cutaneous mastocytosis (CM) into maculopapular mastocytosis or urticaria pigmentosa, diffuse mastocytosis, and mastocytoma or nodular mastocytosis (single or various lesions). The estimated annual incidence of CM is around 0.2 cases per 100,000 population [2]. SM accounts for 10-35% of CM. It may be present at birth or appear within the first 3 months of life (approximately 42-60% of patients), and during the second year of life in most of the remaining cases. It is more common in Caucasian patients, the sex ratio is approximately equal, and most cases are sporadic [3, 4, 5]. The most common presentation is a round or oval, erythematous, yellow-brown or red-brown, indurated macule, papule, or nodule. It usually increases in size over several months and then grows in proportion to the size of the child for a variable period of time. Predilection sites include the trunk and extremities, followed by the head and neck. The lesion may produce hives or blistering when stroked or rubbed (Darier sign) or, more rarely, spontaneously. Darier sign, caused by the release of mast cell mediators induced by physical stimulation, is considered pathognomonic, but its absence does not exclude the diagnosis. Systemic symptoms (flushing, dyspnea, hypotension, nausea, vomiting, etc.) are very rare, and organomegaly and lymphadenopathy are absent [3, 4]. The suspected diagnosis is clinical and is based on the morphology of the lesion, a positive Darier sign, and the absence of systemic involvement. Confirmation diagnosis is by lesion biopsy and histopathological study with metachromatic stains, and immunohistochemical stains with antibodies against tryptase and/or KIT [1, 4]. Differential diagnoses mainly include arthropod bite, bruise, juvenile xanthogranuloma, Spitz nevus, and bullous impetigo [4]. In general, the prognosis is good. Most patients with SM that develop before the first two years of life have a spontaneous resolution before puberty. Treatment is mainly symptomatic. Surgical removal is reserved for isolated patients with accessible lesions and patients with severe symptoms [3, 4, 5]. In our patient, it is possible that the blister was produced by rubbing induced by finger sucking. We decided to excise completely the lesion because it was small and easily accessible.














