Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Cirugía Oral y Maxilofacial
versão On-line ISSN 2173-9161versão impressa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.43 no.3 Madrid Jul./Set. 2021 Epub 25-Out-2021
https://dx.doi.org/10.20986/recom.2021.1315/2021
EDITORIAL
What is the relationship between condylar hyperplasia and temporomandibular dysfunction?
1Director de RECOM. Facultativo Especialista de Área. Hospital Universitario de Badajoz. Badajoz, España
2Práctica Privada, Hospital Quirónsalud Clideba. Badajoz, España
The relationship between condylar hyperplasia and the presence or development of temporomandibular joint (TMJ) dysfunction has been approached very scarcely in the literature. In fact, there are very few clinical series that refer to the coexistence of these two entities and, in most of these few exceptions, the casuistry that refers to this association is lost in the stalemate of data in the results sections of papers involved in the study of TMJ involvement in patients with dentofacial deformity.
Israel1 has recently defined internal derangement (ID) as a condition in which there are damaged intra-articular tissues leading to disturbances in the biomechanical functioning of the TMJ (Figure 1).

Figure 1. Proposed pathway for development of internal derangement of the tempormandibular joint (TMJ).
Based on this broader definition, anterior disc displacement is considered one type of internal derangement without exclusivity. Thus, a patient who has severe limited mouth opening with decreased translation of the TMJ caused by adhesions, osteoarthirtis, synovial inflammation, disc displacement, or other intra-articular disorder is considered to have the clinical signs and symptoms of ID. Besides, condylar hyperplasia (CH) is a non-neoplastic pathology resulting form the excessive growth of the condylar head and neck. It can adversely affect mandibular morphology, dental occlusion, maxillary growth and, which is the focus of our attention in this editorial, the TMJ function.
Some important series have tangentially addressed this clinical association. So, Nitzan et al.2, in a series of 61 patients, reported 40 patients (65.6 %) in which the main complaint was progressive facial asymmetry; 17 (27.9 %) complained of pain, dysfunction, or both. Joint pain, dysfunction, or clicking was found in 24 patients (38.7 %). They stated that the increased functional load may cause contralateral TMJ dysfunction with associated pain and clicking, and concluded that clinicians should be aware that the primary complaint is facial asymmetry in only some patients, and that signs and symptoms of TMJ disease can be present. In a paper from our group3 comprising a series of 36 patients with unilateral CH, we observed that some patients may also present with symptoms from the TMJ such as pain, joint sounds, and limitation of mouth opening. TMJ symptoms were present in 13 out of 36 patients (36 %), involving all clinical types of CH.
Also, in the study by Lippold et al.4, they found that affected joints of patients with CH all have signs of arthrosis in some form, as shown by the histological examination of the condyles (degenerative cartilaginous processes combined with reactive subchondral bony reaction) while these findings were more pronounced in those cases with severe activity in the scintigraphic scans. In the paper by Fushima et al.5, the incidence of TMJ disorders was 33.6 % of total series of patients with malocclusion. In symptomatic subjects, the most frequent sign of TMJ disorders was joint noise (76 %), followed by joint pain (68 %) and disturbance of mandibular movement (38 %). Symmetrical anterior cross bite malocclusion showed low incidence of TMJ disorders. In posterior crossbite malocclusion and mandibular displacement case, however, the signs of TMJ disorders were found frequently. Conclusion was that laleral shift of mandibular head in fossa may relate with the appearance of TMJ disorders.
Also in the series by Elbaz et al.6, among 28 patients with CH type 1 or 2, the temporomandibular disorder was 32.1 %. They concluded that temporomandibular disorder was more frequent in the horizontal form, and that the resultant malocclusion may be an important factor, with the posterior crossbite being particularly harmful to the TMJ. Meanwhile, Ahn and co-workers7, in their study among 63 women, evaluated the influence of internal derangement in facial asymmetry by comparing measurements in cephalograms and MRI to check for disc position. They concluded that TMJ ID, especially when it is more advanced on the unilateral side, can cause mandibular asymmetry, and that the amount of asymmetry did not differed significantly for subjects with bilateral normal TMJs, or with bilateral disc displacement with reduction (DDR), or with bilateral disc displacement without reduction (DDwoR), but only for unilateral cases of TMJ ID with disc displacement.
In the patient with CH, remodelling of the mandibular condyle is mainly related to bone neoformation with displacement of the cephalic portion of the condyle. This scenario changes following condylectomy, which produces a sudden reduction in the intraarticular pressure of both joints. For instance, in the series by Kim et al.8, about 27 patients with unilateral CH undergoing high condylectomy, there was a decrease in the amount of the maximal mouth opening (MMO), but the degree was not severe (about 2.2 mm), and there was an improvement in terms of reduction of joint pain and clicking. Mouallem et al.9 found that condylectomy through a joint interruption did not result in limitation in function, with a 93 % of patients showing normal MMO. In fact, only 6 patients showed a worsening of their pre-op TMJ dysfunction after a condylectomy, but they were only suffering of clicking, without any associated pain.
Also, Niño-Sandoval et al.10, in their systematic review, showed that most of patients suffering presurgical TMJ dysfunction experienced variable results in terms of pain reduction and mandibular function, this illustrating that most series do not specifically deal with management of TMJ dysfunction. However, they concluded that regarding the TMJ after surgical intervention, there was an improvement in pathological condition, and there was no significant TMD complications. Moreover, if we attend to study the incidence of displacement of the disc in patients with dentofacial deformity by MRI, Ooi and colleagues11 found that: 1) DDwoR was present in 56.1 % in class II compared to 19.3 % in class III (p < 0.05); 2) In class III patients, DDwoR was significantly more common in joints with mandibular asymmetry (32.4 %) than in joints with open bite (14.5 %); 3) In class II patients, DDwoR was significantly less common in joints with mandibular asymmetry and without open bite (12.5 %); and 4) DDwoR was only observed on the deviated side in both class III and class II with mandibular asymmetry.
Wolford´s group is among the few ones that have addressed the problem concerning disc position within the TMJ in the patient with CH12. Whenever the disease is active, they always reposition the disc concomitantly with high condylectomy. They studied the evolution in terms of pain reduction and improvement of mouth opening for a group with orthognatic surgery alone compared with the group undergoing high condylectomy plus disc repositioning and orthognatic surgery, and found better results for this last one. Yang's group has also achieved optimal results when repositioning the disc, not by open surgery but by means of arthroscopic suture, referring a 95 % excellent replacement13. This group also used this technique for cases with idiopathic condylar resorption (ICR), demonstrating new bone formation on the condylar head just below the repositioned disc. They concluded that the new anatomical position of the disc favors bone formation over the surface of the degenerated condyle by not completely known reasons, but maybe because of avoiding direct trauma of the posterior slope of the condyle over the temporalis fossa, which has been reported as a possible ethiogenic factor for developing ICR.
In 2009, the arthroscopic technique consisting on performing an anterior myotomy of the upper belly of the pterigoid muscle (which is pushing forward the disc) together with electrocoagulation of areas of synovitis at the bilaminar zone of the posterior ligament (which is responsable for pain) by using ultrasound by coblation was published14. The objective of this technique is to free the disc from its anterior attachment and to generate a retractile tissue in the posterior attachment which may help to get the disc in a posterior fashion while providing its proper mobilization (Figure 2). Whatever open surgery or arthroscopy of the TMJ is performed, it seems that disc reposition is necessary in cases in which TMJ dysfunction persist after treatment of CH (Figure 3).
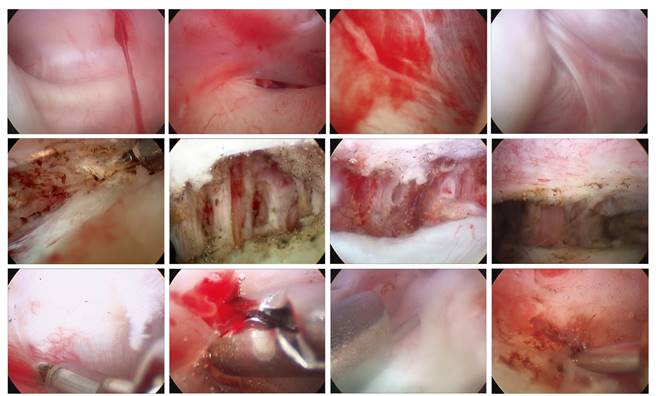
Figure 2. By means of operative arthroscopy, were going to "give a qualitative jump" with respect to arthrocentesis as we are able to visualize the degree of injury inside the joint, such as the degree of synovitis, degree of chnodromalacia, if there are adherences, degree of disc displacement, and if there is a perforated disc, among others. We can perform a myriad of therapeutic maneuvers, such as disc anterior release by miotomy of the lateral pterigoid muscle, electrocoagulation of areas of synovitis with radiofrequency, removal of foreign bodies, subsynovial infiltration of substances such as corticoids, intraluminal instillation of hyaluronic acid, disc suturing or rigid disc fixation with pins.
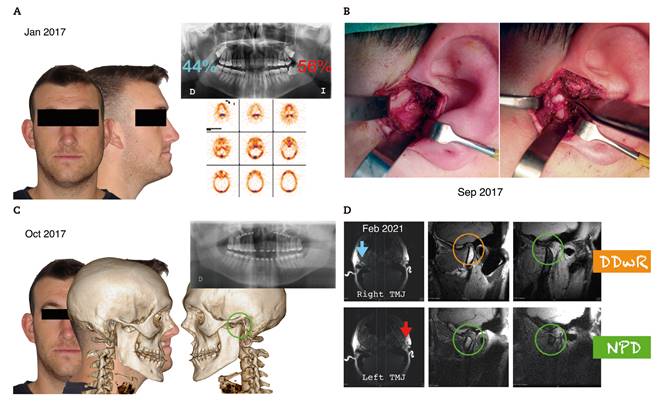
Figure 3 A. This patient came for consultation at 2016 showing a mandibular asymmetry to the right side. The SPECT at January 2017 showed an uptake of 56 % in the left condyle in contrast to 44 % for the right condyle. At September 2017, this difference persisted, and the patient was diagnosed of Type I CH, so he underwent a high condylectomy of the left side. B. We can see the flat remnant condyle and an adequate position of the disc above it, with adequate mobilization. C. Almost a total correction of the asymmetry was achieved, so in October 2019 he underwent a LeFort I osteotomy for advancement of the upper maxilla without mandibular surgery for correction of a dentoskeletal class III in the sagittal plane. D. In February 2021 he developed a closed lock of the right TMJ. MRI showed a normal position of the disc in the left joint in both closed and open mouth, while the disc in the right TMJ was anteriorly displaced with the mouth closed and recaptured when mouth was completely opened. Thus a DDwR of the right TMJ was diagnosed, and the patient underwent an operative TMJ arthroscopy by means of anterior release by miotomy of lateral pterigoid muscle and coblation of the retrodiscal tissues, with an optimal functional outcome.
Unfortunately, we have to conclude that there are still few studies concerning the presence of TMJ internal derangement in patients suffering of CH. However, we hypothesize that these patients may develop a contralateral shift of the TMJ that may promote disc displacement and subsequent compression of retrodiscal tissues that may be responsible for the appearance of TMJ pain, clicking and limited mouth opening. Concerning management, whenever TMJ internal derangement persists after surgical treatment of condylar hyperplasia, operative arthroscopy by means of anterior miotomy and coblation of the retrodiscal tissues must be performed to achieve optimal results in terms of reduction of pain and increase of mouth opening.
BIBLIOGRAFÍA
1. Israel HA. Internal derangement of the temporomandibular joint. New perspectives on an old problem. Oral Maxillofac Sure Clin N Am. 2016;28(3):313-33. DOI: 10.1016/j.coms.2016.03.009. [ Links ]
2. Nitzan DW, Katsnelson A, Bermanis I, Brin I, Casap N. The clinical characteristics of condylar hyperplasia: experience with 61 patients, J Oral Maxillofac Surg. 2008;66(2):312-8. [ Links ]
3. Villanueva-Alcojol L, Monje F, González-García R. Hyperplasia of the mandibular condyle: clinical, histopathologic, and treatment considerations in a series of 36 patients. J Oral Maxillofac Sure. 2011;69(2):447-55. DOI: 10.1016/j.joms.2010.04.025. [ Links ]
4. Lippold C, Kruse-Losler B, Danesh G, Joos U, Meyer U. Treatment of hemimandibular hyperplasia: the biological basis of condylectomy. Br J Oral Maxillofac Surg. 2007;45(5):353-60. DOI: 10.1016/j.bjoms.2006.10.011. [ Links ]
5. Fushima K, Akimoto S, Takamot K, Kamei T, Sato S, Suzuki Y. Incidence of temporomandibular joint disorders in patients with malocclusion. Nihon Ago Kansetsu Zasshi. 1989;1(1):40-50. [ Links ]
6. Elbaz J, Wiss A, Raoul G, Leroy X, Hossein-Foucher C, Ferri J. Condylar hyperplasia: correlation between clinical, radiological, scintigraphic, and histologic features. J Craniofac Surg. 2014;25(3):1085-90. DOI: 10.1097/SCS.0000000000000555. [ Links ]
7. Ahn SJ, Lee SP, Nahm DS. Relationdhip between temporomandibular joint internal derangement and facial asymmetry in women. J Orthod Dentofacial Orthop. 2005;128(5):583-91. DOI: 10.1016/j.ajodo.2004.06.038. [ Links ]
8. Kim JY, Ha TW, Park JH, Jung HD, Jung YS. Condylectomy as the treatment for active unilateral condylar hyperplasia of the mandible and severe facial asymmetry: a retrospective review over 18 years. Int J Oral Maxillofac Surg. 2019;48(12):1542-51. DOI: 10.1016/j.ijom.2019.06.022. [ Links ]
9. Mouallem G, Vernex-Boukerma Z, Longis J, Perrin JP, Delaire J, Mercier J-M, et al. Efficacy of proportional condylectomy in a treatment protocol for unilateral condylar hyperplasia: a review of 73 cases. J Cranio Maxillofac Surg. 2017;45(7):1083-93. DOI: 10.1016/j.jcms.2017.04.007. [ Links ]
10. Niño-Sandoval TC, Araújo Maia FP, Vasconcelos BCE. Efficacy of proportional versus high condylectomy in active condylar hyperplasia. A systematic review. J Cranio Maxillofac Surg. 2019;47(8):1222-32. DOI: 10.1016/j.jcms.2019.03.024. [ Links ]
11. Ooi K, Inoue N, Matshuhita K, Yamaguchi H, Mikoya T, Minowa K, et al. Incidence of anterior disc displacement without reduction of the Temporomandibular Joint in patients with dentofacial deformity. Int J Oral Maxillofac Surg. 2018;47(4):505-10. DOI: 10.1016/j.ijom.2017.11.017. [ Links ]
12. Wolford LM, Morales-Ryan CA, García-Morales P, Pérez D. Surgical management of mandibular condylar hyperplasia type 1. Proc (Bayl Univ Med Cent). 2009;22(4):321-9. DOI: 10.1080/08998280.2009.11928546. [ Links ]
13. Yang C, Cai XY, Chen MJ, Zhang SY. New arthroscopic disc repositioning and suturing technique for treating and anteriorly displaced disc of the temporomandibular joint: part I-technique introduction. Int J Oral Maxillofac Surg. 2012;41(9):1058-63. DOI: 10.1016/j.ijom.2012.05.025. [ Links ]
14. González-García R. Arthroscopic myotomy of the lateral pterygoid muscle with coblation for the treatment of TMJ anterior disc displacement without reduction. J Oral Maxillofac Surg. 2009;67(12):2699-701. DOI: 10.1016/j.joms.2009.07.089. [ Links ]











 texto em
texto em 


