INTRODUCTION
Cutis verticis gyrata (CVG) is a rare benign cutaneous anomaly which is characterised by convoluted folds and furrows of the scalp, mimicking the cerebral sulci and gyri. The folds usually run in an antero-posterior fashion but may also be transverse or mixed. The folds do not flatten on traction or pressure of the scalp. It can be classified as primary essential, primary non-essential and secondary CVG [1]. It is first described in the literature by Robert in 1843 and Unna in 1907 had proposed the name cutis verticis gyrata.
Primary CVG is characterised by normal histopathological appearance of the skin with no associated abnormalities are observed in essential form as opposed to primary non-essential form. Neuropsychiatric and ophthalmic disorder are often described in the latter type, thus procuring the name of Cutis Verticis Gyrata-Intellectual Disability (CVG-ID) syndrome [2]. Secondary CVG occurs as a result of either systemic illnesses, medication or local neoplastic or inflammatory process that cause the pathological scalp changes [1, 3, 4].
CASE REPORT
This is a 33 years old man who presented with hyperpigmented lesion over his scalp since birth. It was initially small, but it grew gradually as the patient aged. The patient was otherwise well with no symptoms such as headache, persistent vomiting, seizure and blurry vision, nor did he complaint of past trauma, pain and discharges from the lesion. Thus, he had not sought treatment in the hospital until recently, as the lesion grew bigger, he had difficulty in wearing his prayer cap as a Muslim believer. There were no significant medical illness and family history with similar condition or consanguinity. Local examination showed a huge hyperpigmented lesion with convoluted folds and furrows resembling cerebriform pattern over the occipital region. The lesion was 16 x 12 cm in size, soft, non-tender and not amenable to traction (Figure 1). There was no palpable cervical lymph node. Systemic examination was normal.
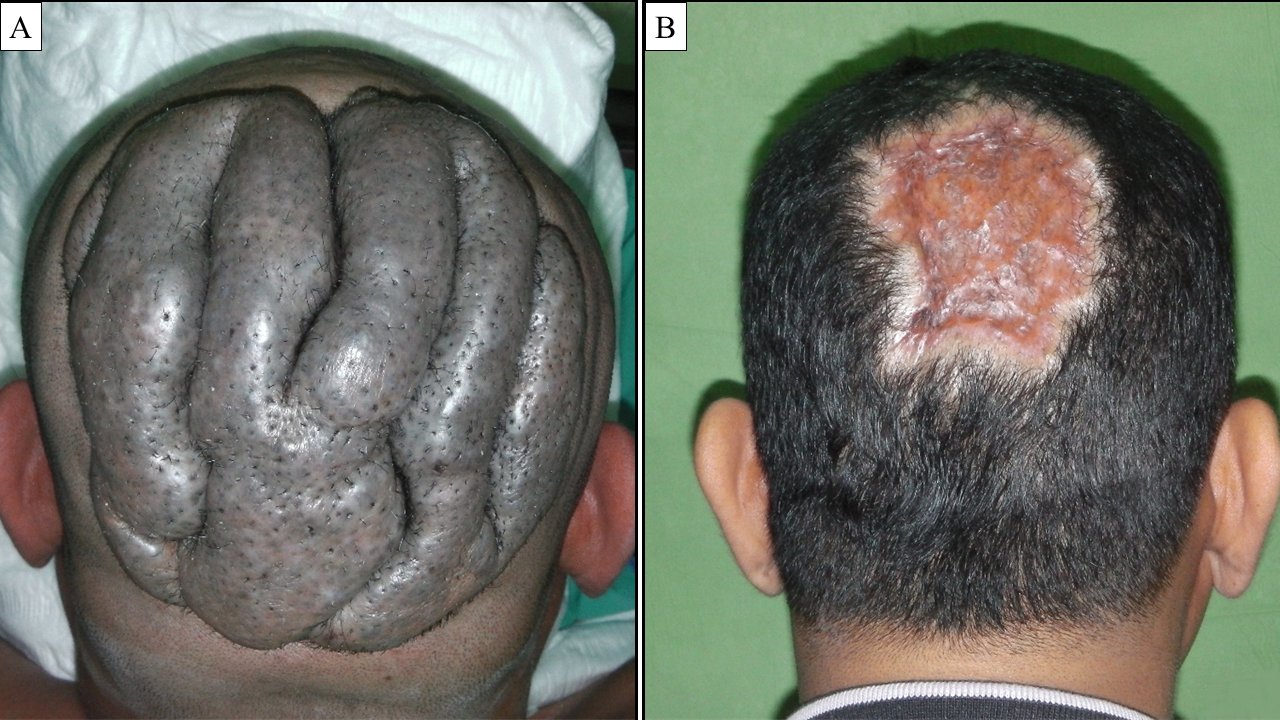
Figure 1. Clinical appearance of the lesion.(A) Pre-operative image showing a 16 cm x 12 cm hyperpigmented lesion with convoluted folds and furrows resembling cerebriform pattern over the vortex and occipital region. (B) One-year post excision and split thickness skin grafting over the scalp.
Computed tomography (CT) scan of the head revealed thickening of the skin and subcutaneous fat with irregular cutaneous fold over the occipital with no intracranial extension. The brain was normal. Excision and scalp reconstruction with split thickness skin grafting was done for the patient under general anaesthesia. Histopathological result had concluded the lesion as completely excised cerebriform intradermal nevus (CIN) with no presence of malignant tissue (Figure 2). The patient was discharged well with no recurrence after 2 years of follow up. He was planned for tissue expander and scalp reconstruction for the alopecia, but the patient was satisfied with the outcome and refused for second surgery. He managed to grow his hair long enough to cover the defect.
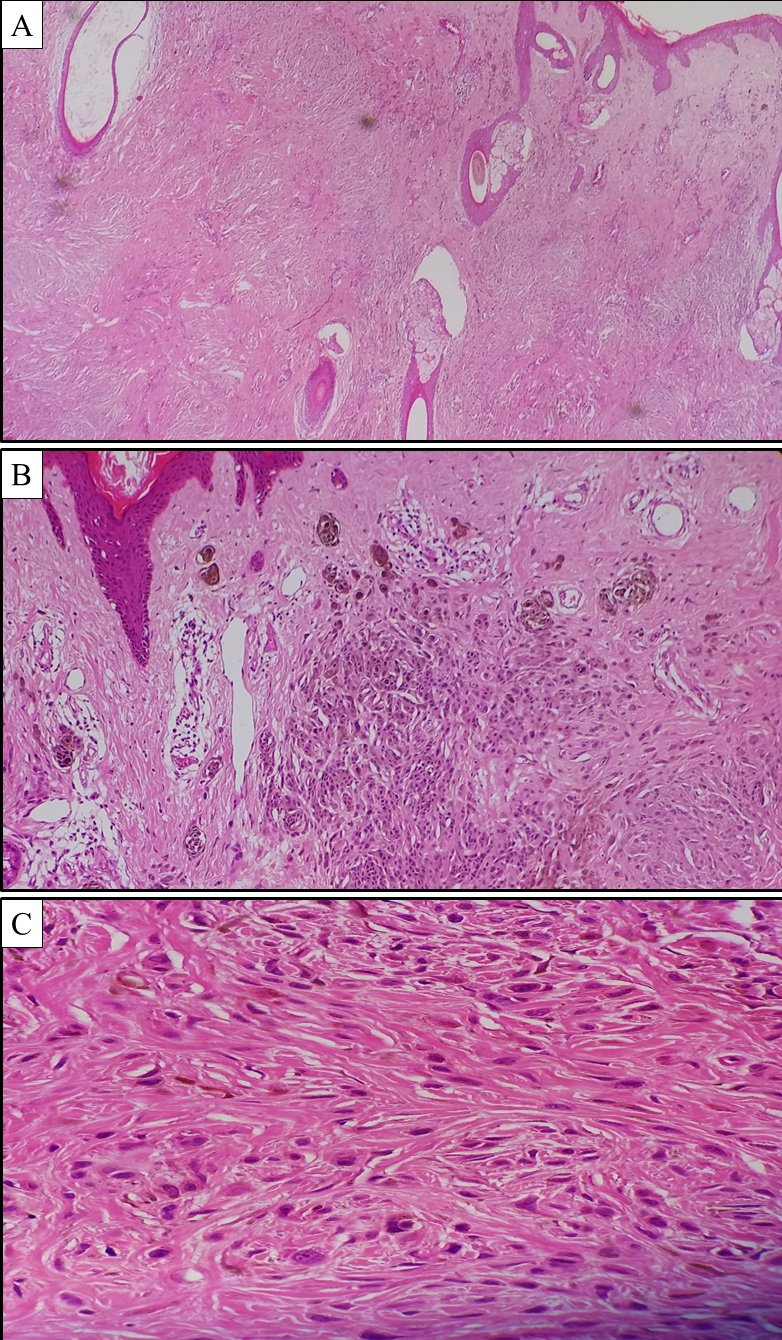
Figure 2. Photo micrograph of the lesion.(A) and (B) The histopathological examination shows symmetrical non-ulcerated intradermal melanocytic proliferation arranged in islands and nests which extend into the adjacent adnexal structures. The epidermis is unremarkable. Areas of atrophic hair follicle with nevoid tissue abutting are prominent in (A). The mid and deeper lesion shows prominent neurotization which resemble neurofibroma can be appreciated in (A). (C) The melanocytes are not associated with atypia or mitotic activity. (A): H&E: 100x; (B): H&E: 200x; (C) H&E: 400x
DISCUSSION
Cutis verticis gyrata (CVG) is a rare morphologic condition comprises ridges and furrows of the scalp that resemble the surface of a brain. It is predominately seen in men, with an estimated prevalence of 1:100000 in males and 0.026:100000 in females [2, 5]. A review of 195 cases of CVG showed a predilection incidence of secondary CVG to primary CVG of 52.3% and 47.7% respectively [1]. Primary CVG is a diagnosis of exclusion, usually seen in post pubertal men before the age of 30 whilst secondary CVG can occur at any age.
The pathophysiology of primary form remains unclear. However, secondary CVG can be caused by various disorders from local inflammatory disease of the scalp such as eczema, psoriasis, impetigo, erysipelas and pemphigus, to local neoplastic changes including melanocytic nevi, dermatofibromas, hamartomas and cylindroma. Systemic disease such as syphilis, tuberous sclerosis, leukaemia, neurofibromatosis, amyloidosis, acromegaly, Ehler-Danlos syndrome, pachydermoperiostosis are also being reported as the secondary association of CVG [1, 6, 7]. As depicted in this case, 25% of secondary CVG is caused by tumour, with dermal nevus being the most common reason.
Cerebriform intradermal nevus, first described by Hammond and Ransom in 1937, is a nodular nevus cerebriform on its surface and intradermal histologically. It is one of the rare forms of congenital melanocytic nevus with preponderance of the female population [8]. Clinically, it usually presents at birth or early life as asymmetric, skin coloured or slightly pigmented tumour over the parietal or occipital scalp. The lesion enlarges gradually and become prominent and demarcated with cerebriform surface. This resultant in progressive alopecia and sparing of hair over the convolutions whilst tufts of hair emerge from the sulci. Recurrent infection and musty odour, pruritus and burning sensation may be presented due to poor scalp hygiene. Patient with CIN will have normal intelligence with no systemic disease observed. It is postulated that hormonal activity may potentiate the growth of the lesions [8]. Nevertheless, the mechanism for the cerebriform pattern on the CIN is unknown.
Diagnosis is based on clinical and histological findings. Histologically, there will be varying amounts of melanin concentrated in the upper dermis. The nest of nevus cell can be well delineated or irregular. Neuroid transformation simulating neurofibroma is seen in the deeper part of the dermis with increased collagen fibers. Hair follicles may appear atrophied with nevoid tissues abutting them. The findings for the histopathology are concurrent with the excised lesion seen in our patient (Figure 2). While CIN is usually benign, there are reported risk of malignant melanoma of up to 10% developed from cerebriform intradermal nevus [7].
The mainstay of the treatment for CIN with CVG is surgical excision and reconstruction in accordance with the reconstructive ladder. Considering the malignant potential of the lesion, complete excision was our priority followed by staged reconstruction of the scalp. The main goal in scalp reconstruction includes functional wound closure to prevent desiccation and infection of the calvarium, as well as cosmetic reason by limiting alopecia and maintaining an appropriate hairline with attention to hair growth patterns. Split thickness skin grafting is a quick, easy and reliable method for medium to large scalp defects as portrayed in our patient. Besides, this method also allows easy monitoring for tumour recurrence, wound contraction and healing for second stage reconstruction of alopecia.
Local flap such as rotational advancement flap can be applied to small to medium size defect. It allows single staged reconstruction with limited alopecia. However, local flap usually requires roughly 4 to 6 times the length of the original defect to accommodate the lack of elasticity of the scalp. Thus, multiple rotational flaps are advocated to distribute the tension over several incision lines especially for medium to large scalp defects [9]. The classical described flaps would be O-to-Z or “pinwheel” flap and Orticochea flap.
The use of tissue expander with local flaps have become the preferred method of secondary scalp reconstruction for larger scalp defects, especially in which local flap cannot provide adequate coverage and the hairline is distorted. Controlled tissue expansion utilised the process of biological and mechanical creep. It can be placed before resection or secondarily after resection once the wound has stabilised. Moehrle et al (2002) has described the implantation of tissue expander in a patient with cerebriform giant melanocytic nevus of the scalp, followed by second stage operation of excision and rotational flap. He also described a different surgical approach in a similar case on different patient via serial excision under subcutaneous slow infiltration tumescent anaesthesia (SITA) before closure with modified mattress sutures “pullet-suture” technique [10]. Both methods require multiple operations but produce excellent cosmetic outcome of limited alopecia. Microvascular tissue transfer is another good alternative for large or total scalp defects especially when the patients have not enough hair-bearing tissue to expand.
CONCLUSIONS
CVG is a rare clinical condition which can be classified into primary or secondary CVG. Proper investigation and aetiology tailored base management should be planned for each individual patient. Cerebriform intradermal nevus is one of the most common causes for secondary cutis verticis gyrata and has the risk of malignant transformation. Surgical excision followed by reconstruction is the mainstay of the treatment.














