Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.3 may./jun. 2006
Analysis of the use of expansion osteotomes for the creation of implant beds. Technical contributions and review of the literature
Análisis del uso de los osteodilatadores para la creación del lecho implantológico. Aportaciones técnicas y revisión de la literatura
Javier Rambla Ferrer 1, Miguel Peñarrocha Diago 2, Juan Guarinos Carbó 3
(1) Master of Oral Surgery and Implantology
(2) Associate Professor of Oral Surgery. Director of the
Master of Oral Surgery and Implantology
(3) Assistant Professor of Oral Surgery.
Valencia University Medical and Dental School. Valencia (Spain)
ABSTRACT
Sometimes, the severe superior maxillary atrophy compromises and even impide oral implants treatment. The use of rotatory instruments (drills) produce heat and lost of bone, but the osteotomes in implantology avoid this and simplifies the surgical treatment allowing implant installation with an easier technique. We present an expansive maxillary technique review, describing the main indications, advantages and disadvantages of this surgical procedure.
Key words: Osteotomes, dental implants, osseous expansion, osseous regeneration.
RESUMEN
La atrofia ósea severa del maxilar superior compromete e incluso, en ocasiones, impide la colocación de implantes. Con la expansión ósea mediante osteodilatadores se evita usar instrumentos rotatorios, no se produce calor ni se elimina hueso y se simplifica el tratamiento quirúrgico permitiendo la colocación de fijaciones sin recurrir a tratamientos más complejos. Presentamos una revisión de la técnica de expansión maxilar mediante osteodilatadores, describiendo las principales indicaciones, ventajas e inconvenientes de este procediminiento quirúrgico.
Palabras clave: Osteodilatadores, implantes dentales, expansión ósea, regeneración ósea.
Concept of bone expansion
Bone expansion in oral surgery consists of expanding atrophic bone crests in order to secure sufficient bone width for dental implant placement. We have conducted an update on this technique with cylindrical expansion osteotomes since the initial descriptions of the procedure by Summers in 1994. A Medline search and examination of the Spanish dental journals have been made in reference to studies on implants placed with expansion osteotomes, to facilitate understanding of the procedure, the concept of bone expansion, and the indications, contraindications, advantages and disadvantages of the procedure. The surgical technique employed is also described.
One of the most common anatomical limitations in oral implantology is bone atrophy of the upper maxilla. Narrow alveolar crests make implant bed preparation difficult, with the appearance of fenestrations or dehiscences of the cortical layers. To avoid these problems, different regenerative surgical techniques have been developed using autologous or homologous bone grafts, xenografts or bone substitutes to allow implant placement in one or two surgical steps (1-4). Chisels have also been used to separate the maxillary cortical components and widen the bone crest the latter in turn being filled with graft material, followed by implant placement one year later (5,6). Nentwing (7) used the same technique, though with immediate implant placement.
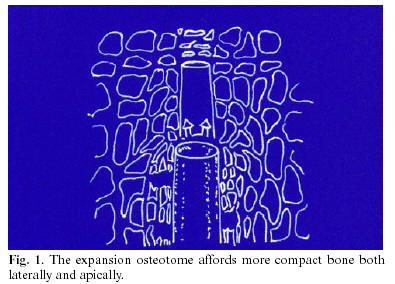
In 1994, Summers (8-10) presented the first cylindrical-conical expansion osteotomes with gradual diameter escalation from one instrument to the next, whereby the base of each instrument corresponded to the active portion of the next instrument. This made it possible to insert the osteotome within the maxillary bone and compress the latter thereby affording increased bone density for the preparation of beds of the same diameter as the required implant (Fig. 1). The apical portion of the instrument is concave, and there are six different diameters marked at different lengths. This instrumentation has modified the implant surgical technique in the upper maxilla due to the existence of more spongy bone, and its anatomical characteristics (Fig. 2).
Since then, different variants of expansion osteotomes have been used, generally in combination with chisels (11-13), expansion screws (14) or other surgical techniques, but always placing the implants in the same intervention (i.e., immediate implant placement). Over time, expansion osteotomes have been applied in the parasinusal angulation technique (15), direct and indirect sinus lift procedures (16,17), and in the placement of implants within the pterygoid region (18,19).
At present, different models of expansion osteotomes are available, based on the design originally developed by Summers but incorporating a number of variations such as the apical tip design or different calibers, that adapt to the implant systems used. Threaded expansion osteotomes have also been developed for application in the upper maxilla and mandible, as well as angulated designs that allow improved access to posterior segments.
Indications and contraindications of expansion osteotomes
In cases with scant bone height, due to the presence of the maxillary sinus, the parasinusal angulation technique can be used (15). This technique takes advantage of the residual bone surrounding the palatal roots of the premolars and molars, and avoids direct approach to the sinus thereby favoring normal osteointegration of the implants.
Expansion osteotomes are used in atraumatic or indirect maxillary sinus floor elevation, fracturing the cortical layer and separating the sinusal membrane. Through the implant bed it is possible to insert small bone particles that in turn facilitate osteointegration of the apical portion of the implant.
Anitua et al. (20) described maxillary bone crest expansion using Summer-type osteotomes, commenting its advantages and inconveniences, and establishing a series of basic indications. The technique is used in situations of bone atrophy, since it allows controlled expansion and avoids undesired deviations by resorting to manual insertion. The use of expansion osteotomes facilitates implant bed preparation at the precise locations defined by the surgical splint.
These instruments are particularly useful in the upper maxilla, since the spongy (or cancellous) bone found in this zone allows perforation, lateral compression and expansion of the adjacent bone. In some cases, in the presence of a degree of resistance, a surgical mallet can be used (20).
The presence of atrophic alveolar crests measuring less than 3 mm in width complicates the placement of implants and makes the complementary use of bone grafts necessary. However, expansion osteotomes do not eliminate bone during bed preparation; rather, the instrument exerts lateral compression, increasing bone density and thus primary implant retention. The placement of implants in narrow maxillary crests in a single surgical step, involving the use of expansion osteotomes, has become a routine, predictable and easy technique (20).
The possibility of anchoring the implants in the external cortical layer of the maxillary sinuses or nasal fossae ensures good primary implant stability. This is referred to as bicortical anchoring, and is achieved thanks to the improved handling performance afforded by manual operation of the expansion osteotomes versus surgical (rotary) drills.
In sinus floor lift procedures, when adopting a direct approach, the mucosa is detached and raised, followed by filling with autologous or heterologous graft material, and placement of the implants in either a second surgical step or in the same intervention depending on the remaining bone available for adequate primary fixation. In these cases, the use of expansion osteotomes for creating the implant bed is indicated as a safe technique that spares bone and facilitates osteointegration of the implants (16).
Expansion osteotomes can be used to place implants in the pterygoid region, where increased control is needed of implant bed inclination in order to avoid damaging the adjacent vascular and nerve elements with the surgical drills (18). Mattsson et al. (21) described the mesiodistal angulation of the implants required to avoid intrusion into the maxillary sinus or nasal fossae without having to resort to implants of shorter length.
Although these instruments are now frequently used, the presence of very dense maxillary bone, or loss of the vestibular or palatine cortical layer, makes it necessary to use other techniques. In patients with antecedents of benign paroxysmal positional vertigo (BPPV), the use of these osteotomes is also disadvised. This form of vertigo is caused by otolith displacements within the posterior semicircular canal of the inner ear, favored by hyper-extension of the head of the patient and the impacts of the surgical mallet. In order to avoid these problems, the patient is to get up slowly after surgery, and excessive tapping with the mallet during surgery should be avoided. If such vertigo appears, the Epley maneuver can be applied, involving hyper-extension of the head with movement towards the side of the affected ear, thereby contributing to reposition the calcium carbonate particles floating within the endolymph compartment. Pharmacological treatment with antivertigo drugs can also be provided (22).
Advantages and inconveniences of expansion osteotomes
The expansion osteotome technique is more conservative in relation to the neighboring structures than conventional drilling (23). Moreover, it affords superior manual control in determining the implant axis thereby contributing to avoid fenestrations and dehiscences. Expansion osteotomes facilitate indirect elevation of the maxillary sinus and nasal fossa, in many cases avoiding the need for more complex bone regeneration techniques. There is also lesser peri-implant bone warming, and no bone loss is produced during expansion (24).
However, tapping of the expansion osteotomes with the surgical mallet is the greatest inconvenience of the technique, and in some cases it may induce BPPV in patients who have experienced no previous episodes of this form of vertigo.
Surgical technique
The basic technique consists of preparing the implant bed by progressively operating the osteotomes until the desired expansion is achieved. Firstly, the alveolar cortical layer is perforated using a rounded drill, followed by insertion of the smallest-caliber osteotome and working up through the successively greater instrument diameters. The expansion osteotomes are inserted manually, pressing and rotating at the same time, until the desired height is reached, or until resistance is encountered. In this situation gentle tapping with the surgical mallet can be applied, rotary instruments can be used (starting with a pilot drill measuring 2 mm in diameter), or even simultaneously operating drills and expansion osteotomes from smaller to larger instrument sizes (25). Except in very spongy bone, use of the surgical mallet is unavoidable.
Once the desired depth has been reached, and before moving on to the next instrument, it is advisable to wait 30-40 seconds for bone microfractures to form and dilate and compact the adjacent bone.
After preparing the bed, we insert the implant immediately, to prevent the socket from collapsing (16,26). Cutting tool insertion is only contemplated in cases of very high bone density (27). Placement of the fixation must be carried out with great care, to avoid fractures or dehiscences of the vestibular table, which in some cases is very thin. Provided they do not compromise primary implant stability, these vertical fractures of the vestibular cortical layer are of no importance, since they consolidate during the osteointegration phase.
On carrying out controlled intrusion or indirect maxillary sinus lifting, a pilot drill is used to create the insertion axis to 2-3 mm from the cortical layer. Percussion with the lesser-diameter expansion osteotomes is then applied until the layer is perforated taking care to avoid damaging the sinusal membrane and the graft material is inserted within the socket (28). This material is displaced apically with the help of larger-diameter instruments, thereby lifting the membrane and compacting the graft material between the latter and the sinus floor. Due to the lack of direct visualization, the technique must be performed with care to avoid perforating the sinusal membrane and inserting the graft material within the sinus.
The expansion osteotome technique can also be used in direct lift procedures, in the presence of a narrow crest that compromises primary implant stability if conventional drills are used (Figs 3 and 4).
Prognosis
The technique of bone expansion with expansion osteotomes offers the possibility of placing implants in cases of bone atrophy without the need for other more complex treatments. In addition, it improves the quality of bone surrounding the implants and reduces the time to rehabilitation (27).
Good gingival esthetic results in the anterior sector require acceptable bone width, and osteotomes are a useful alternative in such situations (29). In posterior sectors, indirect sinus lifting avoids a window approach and allows implant placement in a single stage since the osteotomes compress the apical and lateral bone, thus ensuring primary stability. In addition, it is possible to insert bone substituting grafts through the bed, to increase bone height and allow the placement of implants of greater length (28,30) though no comparative histological studies have yet been made of the bone quality created with osteotomes versus the conventional technique (31).
The first published studies already reported results that served to generate confidence in the procedure (11,20). Thus, Scipioni et al. (32) obtained an average success rate of 98.8% after 5 years of follow-up. Gómez et al. (12) in turn placed 100 implants in 81 patients, using chisels to expand the crest the resulting success rate being 95% during the osteointegration phase.
Komarnyckyj and London (17) placed 16 implants with sinus lift and recorded a 95.3% success rate after two years of follow-up. On the other hand, Rosen et al. (16) studied the survival of 174 implants in 101 patients after 20.2 months of follow-up, and recorded a success rate of 95.4%. In another series of 499 fixations placed with the expansion osteotome technique and sinus lift, the recorded survival rate after two years of follow-up was 97.5% (26).
In 80 patients receiving 158 implants with expansion osteotomes and 68 with the drilling technique, the resulting success rate was 90% and 92%, respectively, after 2.7 years of follow-up (33). The explanation for this minimal difference in performance between the two approaches is that the cases subjected to bone expansion were comparatively less favorable from the start than those amenable to conventional drilling. At present, the success rates of the expansion procedure equal those afforded by conventional drilling. Studies are currently also being made of the use of plasma rich in growth factors (PRGF), combined with the use of expansion osteotomes (34).
In view of the different diagnostic possibilities among patients with maxillary bone atrophy, the management option best suited to each individual case must be applied osteotomes, drilling or direct sinus lifting (35) though the use of osteotomes allows us to deal with situations of extreme bone atrophy without having to resort to more complex techniques.
![]() Correspondence:
Correspondence:
Dr. Miguel Peñarrrocha Diago
Unidad Médico-Quirúrgica
Clínica Odontológica
Gascó Oliag, 1
46021 Valencia
E-mail: miguel.Penarrrocha@uv.es
Received: 30-09-2004
Accepted: 25-03-2005
References
1. Ten Bruggenkate CM, Kraaijenhagen HA, van der Kwast WA, Krekeler G, Oosterbeek HS. Autogenous maxillary bone grafts in conjunction with placement of I.T.I. endosseous implants. A preliminary report. Int J Oral Maxillofac Surg 1992;21:81-4. [ Links ]
2. Pi J. Reconstrucción quirúrgica del maxilar superior atrófico mediante autoinjerto e implantes de titanio puro. Resultados de cuatro años de experiencia. Rev Actual Odontoestomatol Esp 1995;10:37-43. [ Links ]
3. Branemark PI, Adell R, Albrektsson T, Lekholm U, Lindstrom J, Rockler B. An experimental and clinical study of osseointegrated implants penetrating the nasal cavity and maxillary sinus. J Oral Maxillofac Surg 1984;42:497-505. [ Links ]
4. Misch CM, Misch CE. The repair of localized severe ridge defects for implant placement using mandibular bone grafts. Implant Dent 1995;4: 261-7. [ Links ]
5. Osborn JF. Die alveolar extensions plastik. Teil I. Quintessenz 1985; 36:9-16. [ Links ]
6. Osborn JF. Die alveolar extensions plastik. Teil II. Quintessenz 1985; 36:239-46. [ Links ]
7. Nentwig GH. Technique of bone splitting for alveolar recession in anterior maxillary region. Quintessenz 1986;37:1825-34. [ Links ]
8. Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium 1994;15:152, 154-6, 158 passim; quiz 162. [ Links ]
9. Summers RB. The osteotome technique: Part 2. The ridge expansion osteotomy (REO) procedure. Compendium 1994;15:422, 424, 426, passim; quiz 436. [ Links ]
10. Summers RB. The osteotome technique: Part 3. Less invasive methods of elevating the sinus floor. Compendium 1994; 15: 698, 700, 702-4 passim; quiz 710. [ Links ]
11. Faus V. Cresta ósea fina en el maxilar superior. Técnica quirúrgica de dilatación ósea. Rev Esp Odontoestomatol Implant 1994; 4:195-202. [ Links ]
12. Gomez G, Handtmann S, Axmann D, Wuest AK, dHoedt B, Schulte W. La implantación con ensanchamiento simultáneo de cresta alveolar. Quintessence (ed esp) 1996;9:185-94. [ Links ]
13. Nentwig H. Expansión ósea y condensación ósea para mejorar el lecho del implante. Quintessence (ed esp) 1996;9:581-7. [ Links ]
14. López J, Carrera C, Giménez MJ. Expansión ósea de los maxilares con tornillos de osteosíntesis. Rev Esp Oontoestomatol Implant 1996; 4:211-4. [ Links ]
15. Guarinos J, Peñarrocha M, Sanchis JM, Torrella F, Soler F. Tres casos clínicos de la técnica de angulación parasinusal en implantología oral. Quintessence 1997;10:35-9. [ Links ]
16. Rosen PS, Summers R, Mellado JR, Salkin LM, Shanaman RH, Marks MH, et al. The bone-added osteotome sinus floor elevation technique: multicenter retrospective report of consecutively treated patients. Int J Oral Maxillofac Implants 1999;14:853-8. [ Links ]
17. Komarnyckyj OG, London RM. Osteotome single-stage dental implant placement with and without sinus elevation: a clinical report. Int J Oral Maxillofac Implants 1998;13:799-804. [ Links ]
18. Fernández J, Fernández J. Placement of screw type implants in the pterygomaxillary -pyramidal region: surgical procedure and preliminary results. Int J Oral Maxillofac Implants 1997;12:814-9. [ Links ]
19. Nocini PF, Albanese M, Fior A, De Santis D. Implant placement in the maxillary tuberosity: the Summers technique performed with modified osteotomes. Clin Oral Implants Res 2000;11:273-8. [ Links ]
20. Anitúa E. Ensanchamiento de cresta en el maxilar superior para la colocación de implantes: Técnica de los osteotomos. Actualidad Implantológica 1995;7:59-63. [ Links ]
21. Mattsson T, Köndell P, Gynther GW, Fredholm U, Bolin A. Implant treatment without bone grafting in severely resorbed edentulous maxilla. J Oral Maxillofac Surg 1999;57:281-7. [ Links ]
22. Peñarrocha M, Perez M, García A, Guarinos J. Benign paroxysmal positional vertigo as a complication of osteotome expansion of the maxillary alveolar ridge. J Oral Maxillofac Surg 2001;59:106-7. [ Links ]
23. Garg AK. The use of osteotomes: a viable alternative to traditional drilling. Dent Implantol Update 2002;13:33-40. [ Links ]
24. Hahn J. Clinical uses of osteotomes. J Oral Implantol 1999; 25: 23-9. [ Links ]
25. Davarpanah M, Martínez H, Tecucianu JF, Hage G, Lazzara R. The modified osteotome technique. Int J Periodontics Restorative Dent 2001; 21:599-607. [ Links ]
26. Bruschi GB, Scipioni A, Calesini G, Bruschi E. Localized management of sinus floor with simultaneous implant placement: a clinical report. Int J Oral Maxillofac Implants 1998;13:219-26. [ Links ]
27. Roccuzzo M, Wilson T. A prospective study evaluating a protocol for 6 weeks loading of SLA implants in the posterior maxilla. Clin Oral Implants Res 2002;13:502-7. [ Links ]
28. Defrancq J, Vanassche B. Less invasive sinus lift using the technique of Summers modified by Lazzara. Rev Belge Med Dent 2001;56:107-24. [ Links ]
29. Silverstein LH, Kurtzman GM, Moskowitz E, Kurtzman D, Hahn J. Aesthetic enhancement of anterior dental implants with the use of tapered osteotomes and soft tissue manipulation. J Oral Implantol 1999; 25:18-22. [ Links ]
30. Leonetti JA, Rambo HM, Throndson RR. Osteotome sinus elevation and implant placement with narrow size bioactive glass. Implant Dent 2000;9:177-82. [ Links ]
31. Toffler M. Site development in the posterior maxilla using osteocompression and apical alveolar displacement. Compend Contin Educ Dent 2001;22:775-80, 782, 784 passim; quiz 790. Review. [ Links ]
32. Scipioni A, Bruschi G, Calesini G. The edentulous ridge expansion technique: a five-year study. Int J Periodontics Restorative Dent 1994; 14: 51-9. [ Links ]
33. Peñarrocha M, Sanchis JM, Guarinos J, Soriano I, Balaguer J. Estudio comparativo entre la técnica convencional y la de los osteodilatadores para la creación del lecho implantológico. A propósito de 226 implantes colocados en 80 pacientes. Avances en Periodoncia e Implantología 2000;10:189-98. [ Links ]
34. Anitua E. Expansión de cresta con osteotomos: Estado actual. Utilización del plasma rico en factores de crecimiento (P.R.G.F.). Rev Esp Cirug Oral Maxilofac 2001;23:158-62. [ Links ]
35. Fugazzotto PA. Treatment options for augmentation of the posterior maxilla. Implant Dent 2000;9:281-7. [ Links ]











 texto en
texto en